The Renin-Angiotensin-Aldosterone System (RAAS) is a hormone system within the body that is essential for the regulation of blood pressure and fluid balance. The system is mainly comprised of the three hormones renin, angiotensin II, and aldosterone. Primarily it is regulated by the rate of renal blood flow.
This article will describe the system, discuss how the system is regulated, and outline some clinically relevant points around it.
The RAAS
Renin Release
The first stage of the RAAS is the release of the enzyme renin. Renin released from granular cells of the renal juxtaglomerular apparatus (JGA) in response to one of three factors:
- Reduced sodium delivery to the distal convoluted tubule detected by macula densa cells.
- Reduced perfusion pressure in the kidney detected by baroreceptors in the afferent arteriole.
- Sympathetic stimulation of the JGA via β1 adrenoreceptors.
The release of renin is inhibited by atrial natriuretic peptide (ANP), which is released by stretched atria in response to increases in blood pressure.
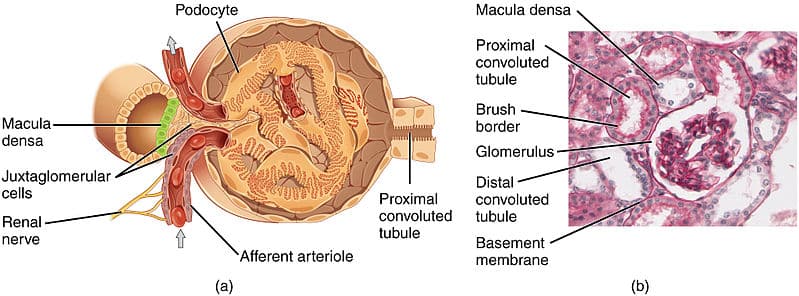
Fig 1 – The juxtaglomerular apparatus demonstrated as a diagram, accompanied by an electron micrograph of it in situ
Production of Angiotensin II
Angiotensinogen is a precursor protein produced in the liver and cleaved by renin to form angiotensin I.
Angiotensin I is then converted to angiotensin II by angiotensin converting enzyme (ACE). This conversion occurs mainly in the lungs where ACE is produced by vascular endothelial cells, although ACE is also generated in smaller quantities within the renal endothelium.
Binding of Angiotensin II
Angiotensin II exerts its action by binding to various receptors throughout the body. It binds to one of two G-protein coupled receptors, the AT1 and AT2 receptors. Most actions occur via the AT1 receptor.
The table below outlines its effect at different points. These will be discussed in more detail below.
| Site | Main Action |
| Arterioles | Vasoconstriction |
| Kidney | Stimulates Na+ reabsorption |
| Sympathetic nervous system | Increased release of noradrenaline (NA) |
| Adrenal cortex | Stimulates release of aldosterone |
| Hypothalamus | Increases thirst sensation and stimulates anti-diuretic hormone (ADH) release |
Effects of Angiotensin II
Cardiovascular Effects
Angiotensin 2 acts on AT1 receptors found in the endothelium of arterioles throughout the circulation to achieve vasoconstriction. This signalling occurs via a Gq protein, to activate phospholipase C and subsequently increase intracellular calcium.
The net effect of this is an increase in total peripheral resistance and consequently, blood pressure.
Neural Effects
Angiotensin II acts at the hypothalamus to stimulate the sensation of thirst, resulting in an increase in fluid consumption. This helps to raise the circulating volume and in turn, blood pressure.
It also increases the secretion of ADH from the posterior pituitary gland – resulting in the production of more concentrated urine to reduce the loss of fluid from urination. This allows the circulating volume to be better maintained until more fluids can be consumed.
Further information on ADH can be found here.
It also stimulates the sympathetic nervous system to increase the release of noradrenaline (NA). This hormone is typically associated with the “fight or flight” response in stressful situations and has a variety of actions that are relevant to the RAAS:
- Increase in cardiac output.
- Vasoconstriction of arterioles.
- Release of renin.
Renal Effects
Angiotensin II acts on the kidneys to produce a variety of effects, including afferent and efferent arteriole constriction and increased Na+ reabsorption in the proximal convoluted tubule. These effects and their mechanisms are summarised in the table below.
| Target | Action | Mechanism |
| Renal artery and afferent arteriole | Vasoconstriction | Voltage-gated calcium channels open and allow an influx of calcium ions |
| Efferent arteriole | Vasoconstriction (greater than the afferent arteriole) | Activation of AT1 receptor |
| Mesangial cells | Contraction, leading to a decreased filtration area | Activation of Gq receptors and opening of voltage-gated calcium channels |
| Proximal convoluted tubule | Increased Na+ reabsorption | Increased Na+/H+ antiporter activity and adjustment of the Starling forces in peritubular capillaries to increase paracellular reabsorption |
Angiotensin II is also an important factor in tubuloglomerular feedback, which helps to maintain a stable glomerular filtration rate. The local release of prostaglandins, which results in preferential vasodilation of the afferent arteriole in the glomerulus, is also vital to this process.
Aldosterone
Finally, angiotensin II acts on the adrenal cortex to stimulate the release of aldosterone. Aldosterone is a mineralocorticoid, a steroid hormone released from the zona glomerulosa of the adrenal cortex.
Aldosterone acts on the principal cells of the collecting ducts in the nephron. It increases the expression of apical epithelial Na+ channels (ENaC) to reabsorb urinary sodium. Furthermore, the activity of the basolateral Na+/K+/ATPase is increased.
This causes the additional sodium reabsorbed through ENaC to be pumped into the blood by the sodium/potassium pump. In exchange, potassium is moved from the blood into the principal cell of the nephron. This potassium then exits the cell into the renal tubule to be excreted into the urine.
As a result, increased levels of aldosterone cause reduced levels of potassium in the blood.
Fig 2 – Diagram outlining the RAAS and its actions on the body.
Clinical Relevance – ACE Inhibitors
ACE inhibitors are a class of drug typically used in the treatment of hypertension and heart failure. Examples include; ramipril, lisinopril, and enalapril.
They inhibit the action of angiotensin-converting enzyme and so reduce the levels of angiotensin II within the body. This means that it reduces the activity of the RAAS within the body. The physiological effects of these drugs, therefore, include:
- Decreased arteriolar resistance
- Decreased arteriolar vasoconstriction
- Decreased cardiac output
- Reduced potassium excretion in the kidneys
These actions help to lower blood pressure in hypertensive patients and also help to improve outcomes in conditions such as heart failure.
Typical side effects include dry cough, hyperkalaemia, headache, dizziness, fatigue, renal impairment, and rarely, angioedema.
Clinical Relevance – Renal Disease
The two most important prognostic factors in chronic kidney disease are hypertension and proteinuria. ACE inhibitors are therefore important in the management of diabetic nephropathy and other forms of chronic renal impairment. This is because they both reduce systemic blood pressure and reduce urinary protein excretion.
The mechanism by which they reduce proteinuria is likely related to the inhibition of the preferential vasoconstriction that occurs in the efferent arteriole in the glomerulus, thus reducing GFR and reducing urinary protein excretion.
It is important to note that ACE inhibitors must be used with caution in patients with bilateral renal artery stenosis and should often be withheld in instances of acute kidney injury, as the reduction in GFR can pronounced and harmful.
