At rest, the heart pumps around 5L of blood around the body every minute, but this can increase massively during exercise. To achieve this high output efficiently, the heart works through a carefully controlled sequence with every heartbeat – this sequence of events is known as the cardiac cycle.
Pressures Within the Heart
| Table 1 – Pressures observed within cardiac chambers during systole and diastole | |
| Heart region | Pressure (mmHg) |
| Right atrium | 0-4 |
| Right ventricle | 25 systolic; 4 diastolic |
| Pulmonary artery | 25 systolic; 10 diastolic |
| Left atrium | 8-10 |
| Left ventricle | 120 systolic; 10 diastolic |
| Aorta | 120 systolic; 80 diastolic |
The above table shows the range of pressures present throughout the heart during the cardiac cycle. Knowing these values can help us understand the progression between different stages of the cycle. For example, the pulmonary artery has a systolic pressure of 25mmHg, so the right ventricle must match this force to successfully eject blood.
The Cardiac Cycle
The cardiac cycle can be divided into four stages:
- Filling phase – the ventricles fill during diastole and atrial systole.
- Isovolumetric contraction – the ventricles contract, but as the heart valves are shut, the volume remains constant. This causes a build-up of pressure, ready to propel blood into the aorta/pulmonary trunk.
- Outflow phase – the ventricles continue to contract as the valves open, pushing blood into the aorta and the pulmonary trunk. This is also known as systole.
- Isovolumetric relaxation – the ventricles relax, ready to re-fill with blood in the next filling phase.
This article will discuss each of the phases in more detail; describing the changes in pressure and the heart valves’ actions in the cardiac cycle.
You can read more on the anatomy of the cardiac valves here.
Filling Phase
The ventricles are filled with blood in two stages – diastole (heart relaxation) and atrial systole (contraction of the atria).
In diastole, both the atria and the ventricles are relaxed. Blood flows from the vena cava and pulmonary veins into the right and left atria respectively, before flowing directly into the ventricles. The ventricles fill with blood at a steadily decreasing rate, until the ventricles’ pressure is equal to that in the veins.
At the end of diastole, the atria contract, squirting a small amount of extra blood into the ventricles. This increases the ventricles’ pressure so that it is now higher than that in the atria, causing the atrioventricular valves (mitral/tricuspid) to close.
Isovolumetric Contraction
As contraction begins both sets of valves are closed, meaning that no blood can escape from the ventricles. Therefore, the start of systole increases the pressure within the ventricles, ready to eject blood into the aorta and pulmonary trunk. The stage of isovolumetric contraction lasts for approximately 50ms, while the pressure builds up.
Outflow Phase
Once the ventricles’ pressure exceeds the pressure in the aorta/pulmonary trunk, the outflow valves (aortic/pulmonary) open and blood is pumped from the heart into the great arteries.
At the end of systole, around 330ms later, the ventricles begin to relax, decreasing ventricular pressure compared to the aorta. This decrease in pressure causes the valves to close. As well as this, blood begins to flow backwards through the outflow valves, which also contributes to the valves’ closure.
Isovolumetric Relaxation
At the end of the outflow phase, both sets of valves are closed once again. The ventricles begin to relax, reducing the pressure in the ventricles so that the atrioventricular valves open. The ventricles then begin to fill with blood, and the cycle begins once again.
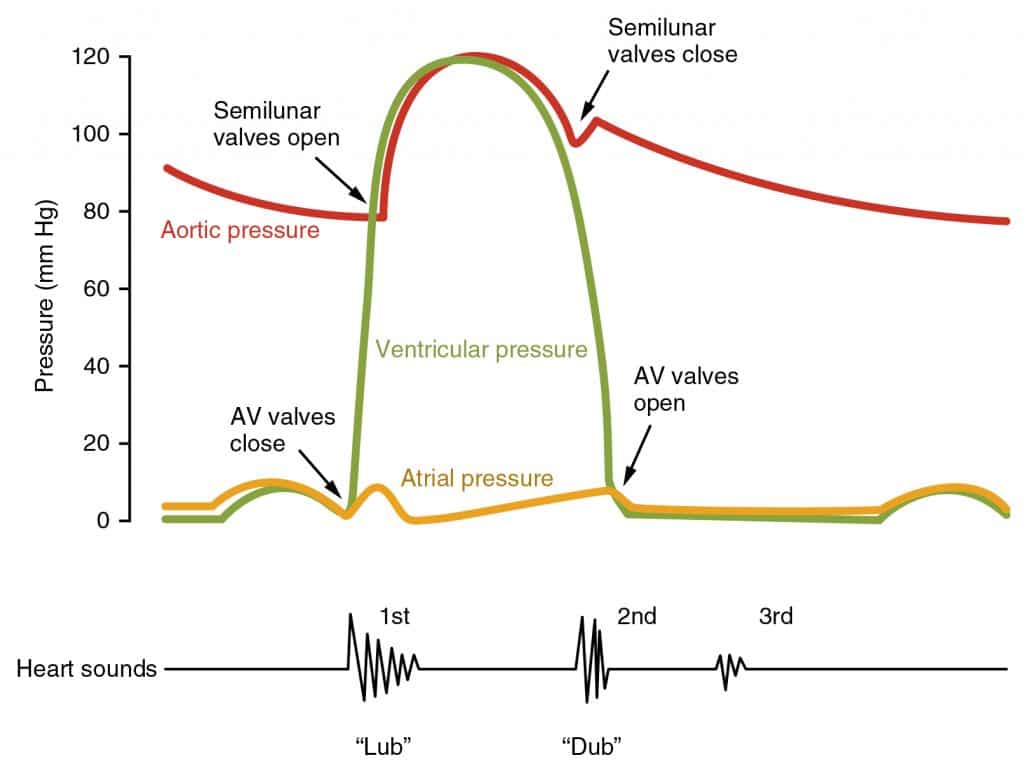
Fig 1 – Pressure changes and important events within the cardiac cycle; a single cycle is shown.
Clinical Relevance – Cardiac Auscultation
The carefully coordinated sequence of events described in this article means that blood flows smoothly in the healthy heart and so cannot be heard on auscultation. When listening to the heart, what can be heard are two sounds, sometimes described as a “lub” and a “dub”. These sounds are caused by the closure of valves in the cardiac cycle:
- S1 (“lub”): occurs at the end of the filling phase when the atrioventricular valves snap shut
- S2 (“dub”): occurs at the end of the outflow phase when the outflow valves snap shut
Damage to the heart valves can cause them to become narrowed (stenosis) or leaky (regurgitation). Either of these conditions can lead to turbulent blood flow which is heard as a humming sound on auscultation of the heart. These sounds are known as heart murmurs.
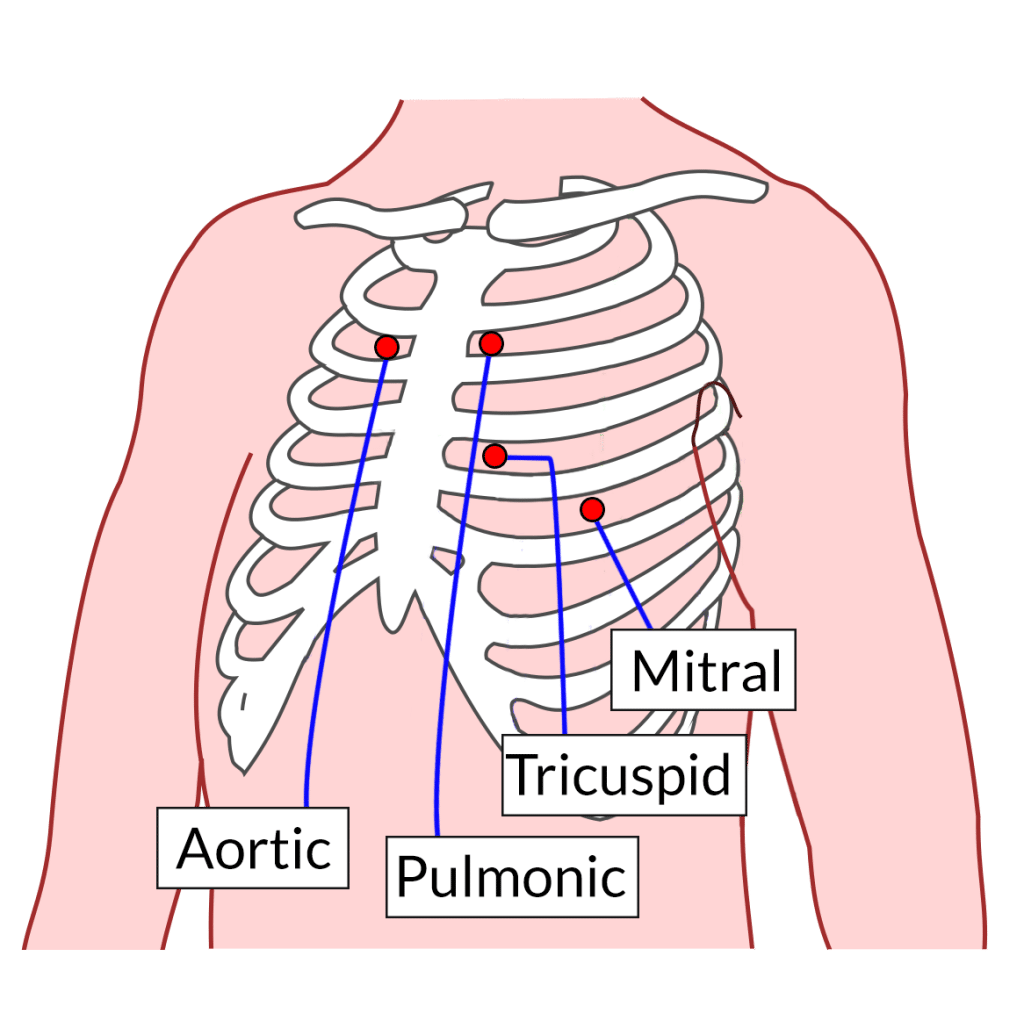
Fig 2 – Diagram showing the sites of auscultation for the cardiac valves
Additional Heart Sounds
Occasionally within clinical practice, additional heart sounds can be heard; these are termed S3 and S4 and can be heard in the following situations:
- S3 : this sound can sometimes be heard early in diastole (following S2). It is normal in young people or athletes; however, it often indicates congestive heart failure in older patients. It is caused by deceleration of blood moving from the left atrium to the left ventricle.
- S4 : this sound can sometimes be heard during atrial contraction (late diastole, immediately before S1) and is associated with reduced ventricular compliance (“stiff” ventricles) or left ventricular hypertrophy.
