A synapse is a gap that is present between two neurones. Action potentials are propagated across the synapse by synaptic transmission, also known as neurotransmission. The neurone that sends the signal is the presynaptic neurone, whilst the postsynaptic neurone receives the signal.
Neurotransmission starts with the release of a readily available neurotransmitter from the presynaptic neurone, followed by its diffusion and binding to the postsynaptic receptors. Then the postsynaptic cell responds according to the neurotransmitter. Following this, the neurotransmitter is removed or deactivated, allowing the entire cycle to occur again.
In this article, we shall look at the stages of synaptic transmission and clinical conditions that arise in its pathology.
Fig 1 – Diagram showing the basic model of neurotransmission. (A) Presynaptic neuron. (B) Postsynaptic neuron. (1) Mitochondria. (2) Synaptic vesicles containing neurotransmitters. (3) Autoreceptor. (4) Synaptic cleft. (5) Neurotransmitter receptor. (6) Calcium channel. (7) Fused vesicle releasing neurotransmitter. (8) Neurotransmitter reuptake pump.
Synthesis and Storage of Neurotransmitters
This is the first step of synaptic transmission. Some neurotransmitters (eg acetylcholine, ACh) are synthesised in the axon, while others (eg neuropeptides) are made in the cell body.
- Acetylcholine – This is synthesised within the synaptic terminal of the axon. Its precursors (choline, acetate) are taken into the cell by membrane channels or created as byproducts of other processes. Enzymes (such as choline acetyltransferase) convert precursors into the neurotransmitter.
- Endogenous opioids (eg. enkephalins) – These are an example of neuropeptides. These large neurotransmitters are produced within the cell body via transcription in the nucleus and translation in the endoplasmic reticulum. Synthesised precursors are then packaged into secretory granules and sent to the axonal terminal. Importantly, proteases present in the granules cleave the precursors into their mature neuropeptide form during this journey.
Once synthesised, neurotransmitters are stored in vesicles within the synaptic terminal until an action potential arrives, causing their release. Neurotransmitters such as acetylcholine are stored within the small synaptic vesicles, whereas neuropeptides reside within large dense-core vesicles.
Neurotransmitter Release
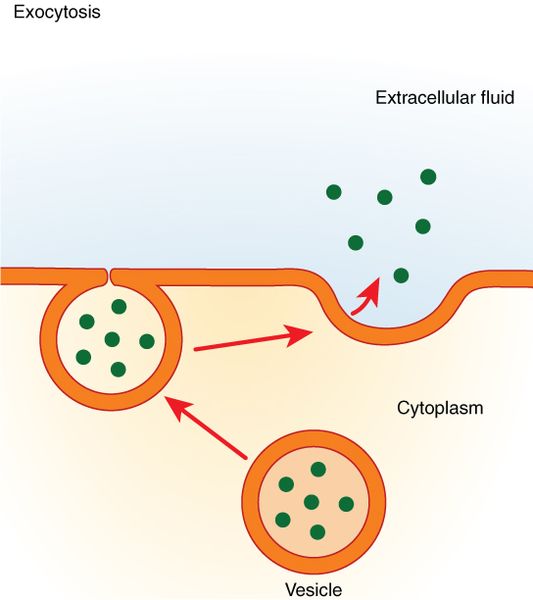
Action potentials depolarising the synaptic terminal lead to the opening of voltage-gated calcium channels. This allows an influx of calcium in the terminal and fusion of the synaptic vesicles with the cell membrane (exocytosis). Consequently, the neurotransmitter is released into the synaptic cleft.
Postsynaptic Receptors
The neurotransmitter in the synaptic cleft diffuses across the gap to the post-synaptic membrane. Here, they can bind to two types of post-synaptic receptors.
| Name | Inotropic receptors | Metabotropic receptors |
| Type | Ligand-gated ion channels | G protein-coupled receptors |
| Response | Channel allows ion flux to change the cellular voltage | Receptor acts through secondary messengers to cause cellular effects |
| Speed of response | Rapid | Slow |
| Length of response | Short-acting | Prolonged response |
This can cause either depolarisation to promote or hyperpolarisation to inhibit the action potential generation in the post-synaptic neurone.
Inactivation/Removal of Neurotransmitters
Once the post-synaptic membrane has responded to the neurotransmitter in the synaptic cleft; it is either inactivated or removed. This can be done in several ways:
- Re-uptake – serotonin is taken back into the pre-synaptic neurone by the transporter proteins in the neuronal membrane. These neurotransmitters are subsequently either recycled by re-packaging into vesicles or broken down by enzymes.
- Breakdown – acetylcholine is broken down by acetylcholinesterase present in the synaptic cleft, inactivating the neurotransmitter.
- Diffusion – into surrounding areas
Clinical Relevance – Acetylcholinesterase Inhibitors
Acetylcholinesterase inhibitors are a class of drug that inhibits the activity of acetylcholinesterase within the synaptic cleft. This increases cholinergic transmission as more acetylcholine is present within the synaptic cleft for longer periods of time.
These drugs, such as pyridostigmine, rivastigmine, and donepezil, can be used to treat various conditions:
- Myasthenia gravis – the inhibition of acetylcholinesterase works at the neuromuscular junction rather than at the synaptic cleft to mitigate the effects of loss of nicotinic acetylcholine receptors.
- Alzheimer’s disease
- Glaucoma
- To reverse the effect of non-depolarising muscle relaxants, such as rocuronium.
As cholinergic transmission is widespread throughout the body, particularly mediating the actions of the parasympathetic nervous system, these drugs can cause many side effects such as bradycardia, hypotension, diarrhoea, excessive salivation or blurry vision.