Antidiuretic hormone (ADH), also known as vasopressin, is a small peptide hormone which regulates the body’s retention of water. It is one of only two hormones secreted by the posterior pituitary gland.
In this article, we will discuss the synthesis, storage, release and action of ADH, and consider its clinical relevance.
Synthesis and Storage of ADH
The synthesis of ADH occurs in the supraoptic and paraventricular nuclei in the hypothalamus. It is then transported to the posterior pituitary gland via the neurohypophysial capillaries. In the posterior pituitary gland, its synthesis is completed and it is stored here until it is ready to be secreted into the circulation.
Release of ADH
The release of ADH is controlled by several factors. The two most influential factors are changes in plasma osmotic pressure, and volume status. Other factors that promote the release of ADH include exercise, angiotensin II, and emotional states such as pain.
ADH release is inhibited by atrial natriuretic peptide (ANP), which is released by stretched atria in response to increases in blood pressure, as well as alcohol and certain medications.
Osmotic Pressure
Osmoreceptorsin the hypothalamus regulate the amount of ADH released in response to changes in the osmotic pressure of plasma. They are located in the organum vasculosum of the lamina terminalis (OVLT) and the subfornical organ, which are two of the sensory circumventricular organs of the brain. Both organs lack a blood-brain barrier, allowing them to directly detect the osmolarity of the blood.
Osmotic pressure is dependent on the plasma osmolality. Plasma osmolality is in turn affected by the total body plasma volume. Following a fall in plasma volume there is an increase in the plasma sodium (Na+) concentration, and therefore the osmolarity is increased.
Subsequently, water exits cells, and moves down its concentration gradient into the plasma. This stimulates the osmoreceptors cells to contract, which results in afferent signals being sent from the hypothalamus to the posterior pituitary gland to increase the release of ADH.
Alternatively, if there is an increase in the total body volume then the osmolality of the plasma will reduce. In this situation, water will move down its concentration gradient from the plasma, into osmoreceptor cells, causing them to expand. As a result, afferent signals are sent from the hypothalamus to the posterior pituitary gland to decrease the release of ADH.
Volume Status
ADH secretion also occurs during states of hypovolemia. Baroreceptors in the left atrium, carotid artery and aortic arch detect changes in arterial blood volume.
If blood pressure reduces, baroreceptors relay this to the vagus nerve, which sends afferent signals that directly stimulate the release of ADH from the posterior pituitary. Conversely, in a hypervolemic state, the release of ADH will be reduced.
Action of ADH
The main action of ADH in the kidney is to regulate the volume and osmolarity of the urine. Specifically, it acts in the distal convoluted tubule (DCT) and collecting ducts (CD).
During states of increased plasma osmolality, the secretion is increased. ADH acts through a G-protein coupled receptor to increase the transcription and insertion of aquaporin–2 channels to the apical membrane of the DCT and CD cells. Consequently, the permeability of the DCT and CD cells to water increases.
This allows water to move down its concentration gradient, out of the nephron and back into the bloodstream, thus normalising plasma osmolality and increasing total blood volume.
In response to decreased plasma osmolarity, ADH release is reduced. This reduces the number of aquaporin-2 channels being inserted into the apical membrane of the DCT and CD cells. In turn, there is a subsequent reduction in the amount of water reabsorbed from the nephron back into the bloodstream.
In high concentrations, ADH can also act on the blood vessels to increase peripheral vascular resistance, the result of which is increased blood pressure. This mechanism is useful in restoring blood pressure during hypovolemic shock.
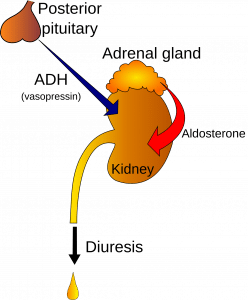
Fig 1 – Diagram showing the ADH axis
Clinical Relevance – Diabetes Insipidus
This condition is characterised by excessive thirst and secretion of copious amounts of dilute urine. It is usually diagnosed by the presence of high plasma osmolality and low urine osmolality. A water deprivation test can help with diagnosis. There are two different types of diabetes insipidus:
- Cranial diabetes insipidus – occurs due to a lack of secretion of ADH from the posterior pituitary gland. This could be idiopathic, or possibly due to damage to the pituitary gland by tumours, infection or trauma. It is treated with ADH analogues.
- Nephrogenic diabetes insipidus – there is no impairment in the release of ADH from the pituitary gland. However, the kidney is unable to respond to the ADH and remove water from the urine. Causes include genetic predisposition, electrolyte disturbances and some medications (e.g. lithium). Management of the condition is difficult, but methods such as high-dose ADH analogues, thiazide diuretics, amiloride and NSAIDs can be trialled.
Clinical Relevance – Syndrome of Inappropriate ADH (SIADH) secretion
SIADH is characterised by hyponatraemia secondary to excessive retention of free water. Symptoms can be mild, but in severe cases, cerebral oedema and resultant neurological dysfunction can occur. Common causes of SIADH include:
- Malignancy e.g. small cell lung cancer
- Brain injury e.g. stroke or subarachnoid haemorrhage
- Infections e.g. atypical pneumonia, meningitis
- Drugs e.g. carbamazepine, sulfonylureas
When treating SIADH care must be taken to correct Na+ slowly, to avoid precipitating a severe neurological sequelae – cerebral pontine myelinolysis. The mainstay of management is fluid restriction, although in some cases demeclocycline may be used.
