Ventilation is the movement of air in and out of the lungs which facilitates gas exchange. It occurs via the respiratory muscles, which contract and relax rhythmically to fill the lungs with air during inspiration and empty them in expiration. This article will discuss the neural control of ventilation and its clinical relevance.
Involuntary control
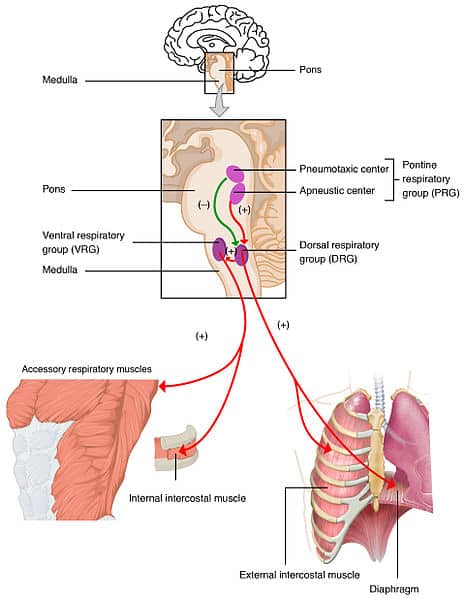
Involuntary respiration is under subconscious control. The diaphragm and intercostal muscles are the primary respiratory muscles. They are stimulated by groups of neurons located in the pons and medulla. These neurons form the respiratory control centre. They send impulses to the primary respiratory muscles, via the phrenic and intercostal nerves, which stimulate their contraction. There are three main groups of neurons involved in respiration:
- The ventral respiratory group controls expiration
- The dorsal respiratory group controls inspiration
- The pontine respiratory group controls the rate and pattern of breathing
Once the neurons stop firing, the inspiratory muscles relax and expiration occurs.
Further information on the mechanics of breathing can be found here.
Voluntary Control
Voluntary respiration is under conscious control. It is controlled via the motor cortex in the cerebrum, which receives inputs from the limbic system and hypothalamus. The mechanisms involved aren’t completely understood, but signals are thought to be sent to the spinal cord from the motor cortex, which are then passed onto the respiratory muscles.
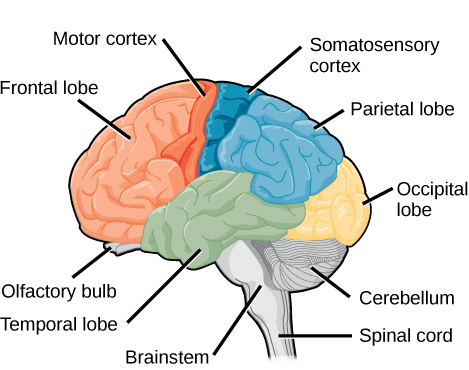
Fig 2 – Regions of the brain, neurons in the motor cortex are responsible for voluntary control of respiration.
Clinical Relevance – Phrenic nerve paralysis
Phrenic nerve paralysis is where damage to the phrenic nerve results in its dysfunction. This can cause paralysis of the diaphragm, therefore causing breathing problems. Patients may lose the ability to regulate their own breathing.
Common causes include: spinal cord injury, neck injury and surgical complications.