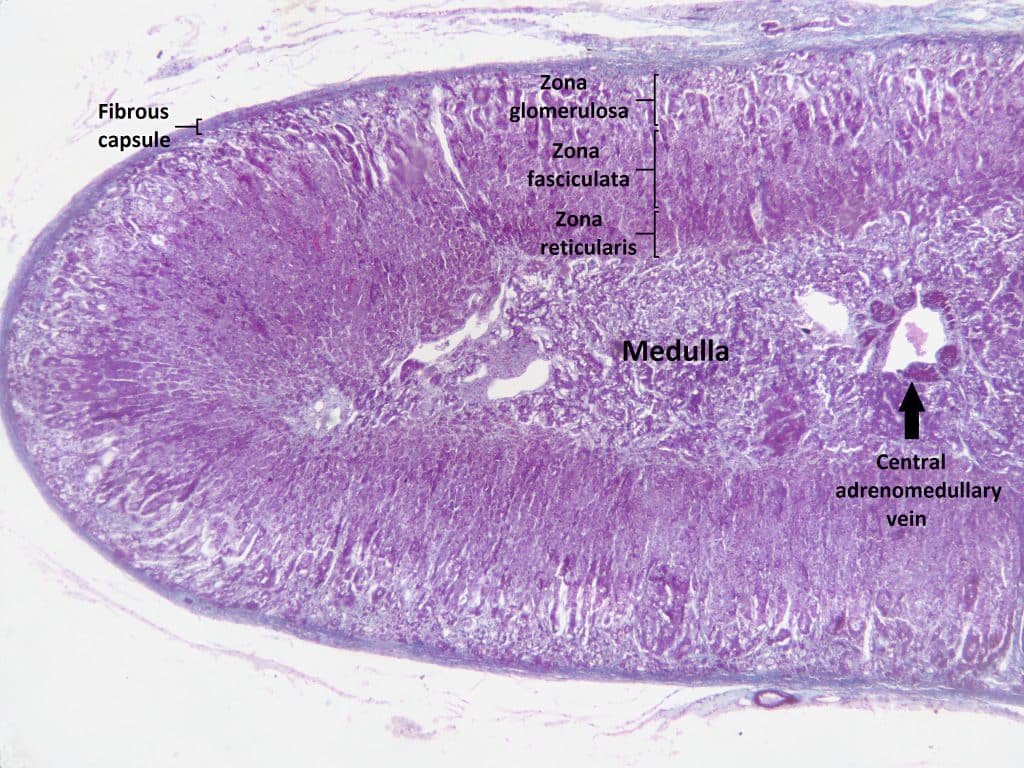
The zona fasciculata is the middle zone of the adrenal cortex, deep to the zona glomerulosa and superficial to the zona reticularis. It is the thickest of the three adrenal layers, measuring approximately 0.9mm and making up 50% of the mass of the adrenal gland.
In this article, we will discuss the cellular arrangement, function and clinical relevance of the zona fasciculata.
Structure
The zona fasciculata is made up of parenchymal cells known as spongiocytes, arranged into columns (sometimes called fascicles) with venous sinuses in between.
Blood flows into the adrenal gland from the adrenal arteries, which are branches of the phrenic and renal arteries as well as the aorta. From here, blood flows through the adrenal tissue from superficial to deep, draining into sinusoids in the adrenal medulla and eventually into the central adrenal vein.
Function
The cells of the zona fasciculata secrete the glucocorticoids cortisol and corticosterone. These hormones regulate carbohydrate metabolism, particularly when an individual is in a time of stress (as part of the “fight-or-flight” response).
In an adult human, approximately 10mg of cortisol and 3mg of corticosterone are secreted over a 24-hour period.
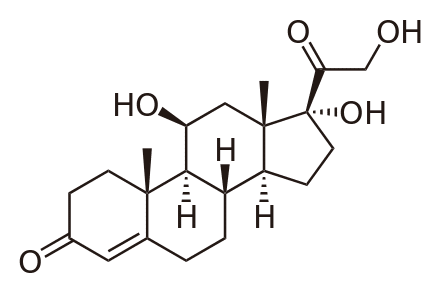
The synthesis pathway of the steroids secreted by the zonas of the adrenal gland is complex. Cholesterol is the major precursor for all steroids secreted.
The first step is initiated by the actions of ACTH and angiotensin II activating adenylyl cyclase and phospholipase C respectively. Cholesterol can then be converted to a steroid called pregnenolone via an enzyme of the cytochrome P450 superfamily called cholesterol desmolase.
From pregnenolone, all the major secreted mineralocorticoids, glucocorticoids and androgens can be synthesised in a multi-step enzyme-assisted pathway. The metabolites of the synthesis pathway are moved in and out of the mitochondria, the smooth endoplasmic reticulum and the cytoplasm.
It is the presence or lack of specific enzymes in each zona that determines which hormones are secreted. In the zona fasciculata, the enzyme 11β-hydroxylase catalyses the final step of the reaction that forms cortisol and corticosterone.
Additionally the secretion of cortisol follows a diurnal pattern with more being secreted in the mornings.
Clinical Relevance – Cushing’s Syndrome
In a steroid-producing adrenal tumour (or anterior pituitary adenoma), large concentrations of glucocorticoids are secreted in the body. When in high concentrations, glucocorticoid steroids activate mineralacorticoid receptors due to the similarity in shape of the receptors.
Therefore, a patient with Cushing’s Syndrome will have symptoms of high glucocorticoid secretion (fat build-up on back of neck and around face, wasting of limb muscles with central obesity, purple striae, hyperpigmentation) as well as effects of high mineralocorticoid concentrations (hypertension, hypokalaemia).
Treatment of Cushing’s depends on the underlying cause, for example a pituitary adenoma may be surgically removed, as can a metastatic lung tumour secreting ACTH.
Clinical Relevance – Enzyme Deficiencies
A deficiency in the enzyme 3β-hydroxysteroid dehydrogenase causes an increased secretion of DHEA – a weak androgen that causes masculinisation in females but is not strong enough to drive male genital development alone. As such, male neonates with this deficiency are likely to have hypospadias, where the opening of the urethra is found on the underside of the penis rather than at the tip.
The most common adrenal enzyme deficiency is 21β-hydroxylase deficiency, making up 90% of the deficiency cases. Production of Cortisol and Aldosterone are reduced, causing a raised ACTH secretion. Precursor steroids are converted to androgens which then drive masculinisation, although this may not become apparent until later life. The lack of aldosterone results in massive loss of Na+ which manifests as severe hypovolaemia.