Haematopoiesis describes the production of cells that circulate in the bloodstream. Specifically, erythropoiesis is the process by which red blood cells (erythrocytes) are produced.
On average, the body produces an astounding 2.5 billion red cells/kg/day. Erythrocytes arise from a complex line of cells, and their rate of production is tightly regulated to ensure adequate but not excessive numbers of red blood cells are produced.
In this article, we will consider the stages and regulation of erythropoiesis, and review what happens when it goes wrong.
Sites of Erythropoiesis
The site of erythropoiesis changes throughout life. In the very early foetus, it occurs in the yolk sac. From 2 – 5 months gestation, it occurs in the liver and spleen before finally establishing in the bone marrow from about 5 months gestation.
In children, erythropoiesis can occur in the bone marrow of most bones. However, in adults, it only occurs in the bone marrow of the vertebrae, ribs, sternum, sacrum, pelvis and proximal femur.
When erythropoiesis is inadequate in the bone marrow, this can trigger extramedullary haematopoiesis – i.e. haematopoiesis occurring outside the marrow. This is commonly seen in haemoglobinopathies such as thalassaemias and myelofibrosis.
Stages of Erythropoiesis
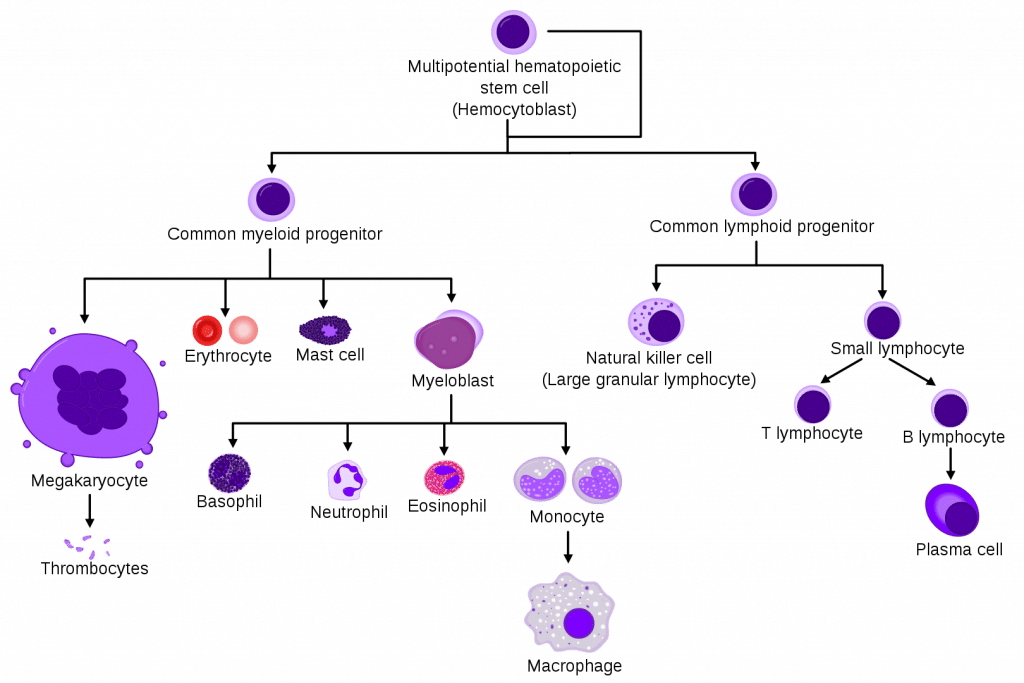
The production of all blood cells begins with the haemocytoblast, a multipotent haematopoietic stem cell. Haemocytoblasts have the greatest powers of self-renewal of any adult cell. They are found in the bone marrow and can be mobilised into the circulating blood when needed.
Some haemocytoblasts differentiate into common myeloid progenitor cells, which go on to produce erythrocytes, as well as mast cells, megakaryocytes and myeloblasts.
The process by which common myeloid progenitor cells become fully mature red blood cells involves several stages. First, they become normoblasts (aka erythroblasts), which are normally present in the bone marrow only.
Then, they lose their nucleus as they mature into reticulocytes, which can be thought of as immature red blood cells. Some of these are released into the peripheral circulation.
Finally, reticulocytes lose their remaining organelles as they mature into erythrocytes-which are fully mature red blood cells. the average lifespan of a red blood cell is approximately 120 days.
During this maturation process, there is nuclear extrusion – i.e. mature erythrocytes have no nucleus. Nucleated red blood cells present in a sample of bone marrow can indicate the release of incompletely developed cells. This can occur in pathology such as thalassaemia, severe anaemia or haematological malignancy.
Regulation of Erythropoiesis
Erythropoiesis is driven mainly by the hormone erythropoietin (EPO), which is a glycoprotein cytokine.
EPO is secreted by the kidney. It is constantly secreted at a low level, sufficient for the normal regulation of erythropoiesis. However, if the erythrocyte level becomes inadequate, the blood becomes relatively hypoxic. When there is a reduced partial pressure of oxygen (pO2) in the kidney, this is detected by the renal interstitial peritubular cells.
In response, there is a surge in EPO production, which acts on the bone marrow to stimulate increased red blood cell production. This causes haemoglobin levels to increase, subsequently causing the pO2 to rise and therefore EPO levels to fall. The feedback loop is complete.
Clinical Relevance – Chronic Kidney Disease
Chronic kidney disease often causes anaemia. In the damaged kidney, there is a reduced basal level EPO production and a reduced response to hypoxia leading to anaemia. To counteract this, patients can be given EPO injections as required.
Clinical Relevance – Drug Doping
Exogenous EPO can be used as a performance-enhancing drug among athletes. By stimulating increased red blood cell production, it increases the amount of haemoglobin available for oxygen binding, thus improving the oxygen supply to muscles. However, studies have disagreed over whether this translates to enhanced athletic performance.
Clinical Relevance – Underproduction of Red Blood Cells
The underproduction of red blood cells results in anaemia. Anaemia is defined as a low haemoglobin concentration, but the absolute values differ between women and men.
In broad terms, anaemia can be caused by decreased red cell production, or increased red cell removal. Here we will briefly consider the causes of decreased red cell production.
Reduced red cell production may be due to 3 main things:
- Lack of ‘building blocks’ for production, e.g. iron, folate or B12 deficiency.
- Failure of the stimulus – i.e. EPO deficiency secondary to chronic kidney disease.
- Bone marrow failure, such as aplastic anaemia.
Clinical Relevance – Overproduction of Red Blood Cells
Overproduction of red blood cells can occur in conditions such as polycythaemia rubra vera. This is a myeloproliferative disease which results from dysregulation at the level of the haematopoietic stem cell.
Even though EPO production is switched off, excess red blood cells are continually produced. Over 95% of patients with polycythaemia are positive for the JAK-2 mutation, and it usually affects patients over the age of 60. Usually, patients remain well with the disease for many years, however, it can cause an increased risk of thrombosis, and around 3% of cases transform into acute leukaemia- therefore, regular monitoring is vital.