A number of physiological responses take place when the respiratory system is placed under stress. This article will focus on the responses of the respiratory system to exercise and being at an altitude, and end by discussing its clinical relevance.
Exercise
During exercise, the gas exchange requirements of the lung increase due to increased oxygen consumption and increased carbon dioxide production. In addition, both the respiratory rate and tidal volume increase, hence alveolar ventilation also increases. This increases the rate of gas exchange and minute volume. It is not fully understood why the ventilation rate increases when exercising and several mechanisms are thought to be implicated.
There are also cardiac changes; an increase in heart rate and stroke volume causes an increase in cardiac output. This results in an increase in pulmonary circulation. Blood flow is redistributed, with more blood being directed to the middle and upper zones via the recruitment of more pulmonary capillaries. This leads to reduced regional differences within the lung.
Intense exercise also results in increased lactic acid production.
Anaerobic Exercise
Exercise can be aerobic or anaerobic. The term anaerobic threshold (AT) is used to describe the point at which anaerobic metabolism begins.
During aerobic respiration, carbon dioxide production, minute volume and alveolar ventilation increase proportionally, resulting in a constant pCO2. However, after the AT, the minute volume and alveolar ventilation rate increase more than the CO2 production, leading to a low pCO2. Anaerobic metabolism also increases lactic acid production and the point at which this occurs will vary with the fitness of the individual. This can result in hyperventilation and lactic acidosis.
Oxygen Consumption
As work increases, oxygen consumption (Vo2) increases proportionally until it plateaus. This plateau occurs at the AT. Oxygen consumption is at a maximum (VO2 max), and oxygen uptake remains at this point because it is not possible to further increase the cardiac output. This maximum point is approximately 10 times the resting oxygen consumption.
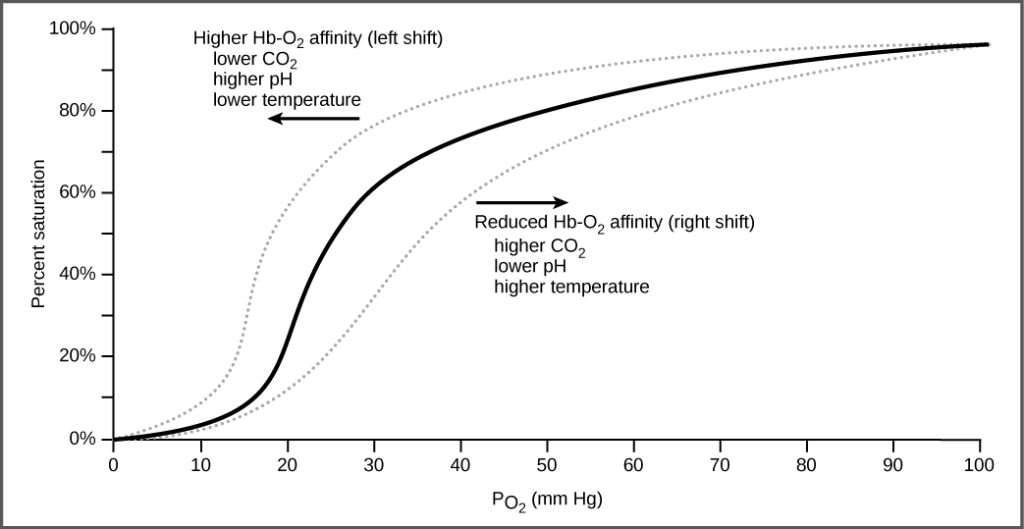
In the oxyhaemoglobin dissociation curve, exercise causes a right shift due to the increased body temperature, pCO2 and [H+]. This increases oxygen availability to the muscles.
At Altitude
As altitude increases, atmospheric pressure decreases. At sea level, atmospheric pressure is approximately 760mmHg (compared to approximately 253mmHg at the peak of Mount Everest). These atmospheric pressures can be used to calculate the partial pressure of oxygen (pO2) in air. This shows that the pO2 is approximately 159mmHg at sea level and 43mmHg at the summit of Mount Everest.
Acclimatisation
Acclimatisation describes the normal physiological changes through which the body adapts to decreasing levels of oxygen. It explains why in parts of the world such as Tibet, many generations of people have lived at high altitude whereas climbers have to take considerable care when moving to high altitudes.
Hyperventilation is one of the most notable manifestations of acclimatisation. This occurs when peripheral chemoreceptors detect a decrease in arterial pO2 and increase the respiratory rate to compensate. This can result in hypocapnia and alkalosis. These initially prevent a further increase in respiratory rate due to CO2 being sensed by the central chemoreceptors in the cerebrospinal fluid (CSF) by removing carbon dioxide. However, after a few days, the pH of the CSF and arterial blood are returned to normal following a response from the CSF and kidneys involving bicarbonate ions. This, therefore, means that the respiration rate can continue to increase.
It is also important to mention 2,3-Biphosphoglycerate (2,3-BPG). This is formed during glycolysis in the red blood cell. It binds to one of the beta chains of the haemoglobin, allowing deoxygenation and a right-hand shift of the oxyhaemoglobin curve. The respiratory alkalosis resulting from hyperventilation at altitude leads to a rise in 2,3-BPG after a couple of days, which contributes to decreased oxygen in the blood.
Polycythaemia is an increase in haematocrit. This is a feature of acclimatisation that is much slower to develop. It can have a number of causes, but in the case of people at high altitudes, the cause is an increase in the number of circulating red blood cells. It is important to note that whilst at altitudes, polycythaemia is an appropriate physiological response. However, it causes hyperviscosity which can become pathological.
In response to hypoxia, the kidney releases the hormone erythropoietin which stimulates red cell production in the bone marrow. This results in increased haemoglobin levels, hence an increased capacity to carry oxygen.
Clinical Relevance – Altitude Sickness
Altitude sickness, also known as acute mountain sickness, results from acute exposure to low partial pressure of oxygen at high altitudes. It can present with a number of symptoms, including:
- Headaches
- Nausea and vomiting
- Shortness of breath
- Tachycardia
- Peripheral oedema
- Pulmonary oedema
Ascending to very high altitudes rapidly can often make this worse. The best way to prevent it is by ascending slowly and avoiding strenuous activity in the first 24 hours after ascending. In severe cases, the only reliable treatment is to descend from the altitude. Oxygen supplementation and steroids can sometimes be used to treat the symptoms.