The brain requires a large amount of oxygen and glucose to meet its high metabolic demand. Therefore, cerebral circulation has structural and functional adaptations to ensure a consistently high blood flow is maintained. Any interruption to this blood flow can cause a loss of consciousness in a few seconds and irreversible damage to neurons after 4 minutes.
This article will explore the structural and functional adaptations of the brain’s circulation.
Structural Adaptations
Circle of Willis
The circle of Willis is anastomoses (that is, multiple direct connections between arteries) between the basilar and internal carotid arteries. It provides collateral blood flow, protecting the brain against ischaemia. This means that even if one artery is damaged, blood flow is not compromised.
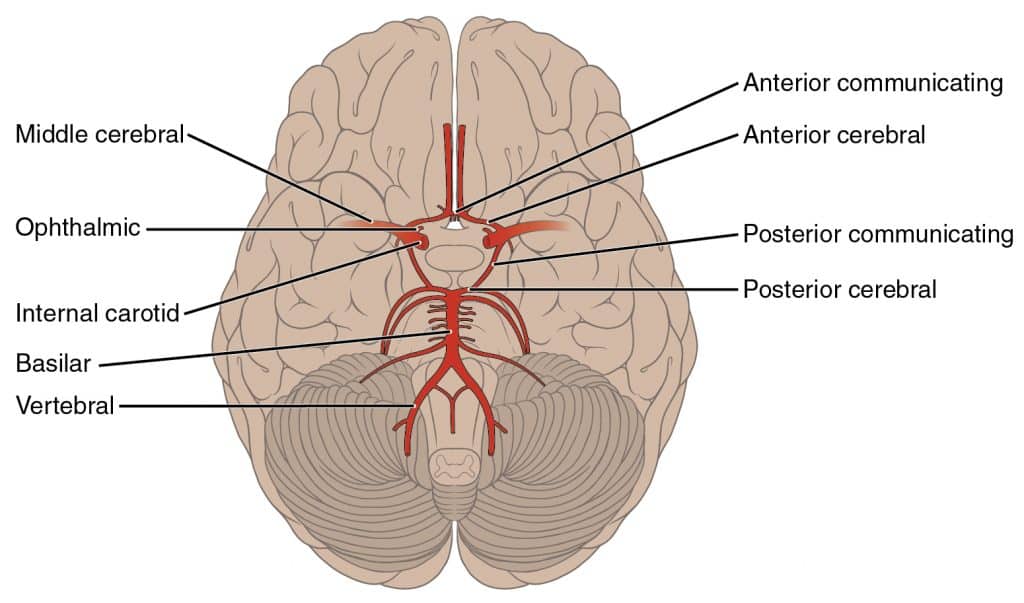
Fig 1 – Circle of Willis makes up the arterial supply to the brain and is formed by anastomosing arteries
Blood-brain barrier
The blood-brain barrier is a highly selective barrier between the systemic circulation and the brain’s extracellular fluid. It is formed by four structures: capillary endothelial cells, basement membrane, pericytes and projections from astrocytes. It is permeable to lipid-soluble molecules such as O2 and CO2 and impermeable to lipid-insoluble molecules like K+ and catecholamines. Its main function is to protect the brain from harmful neurotoxins and to prevent infections from spreading to the brain and causing encephalitis.
Functional Adaptations
Myogenic Autoregulation
This mechanism regulates local blood flow to the brain by allowing the blood vessel diameter to change with blood pressure. When blood pressure rises, vasoconstriction occurs to reduce blood flow. This protects the smaller vessels from rupturing because of the high pressure. When blood pressure decreases, vasodilation occurs to increase blood flow. This stops the blood pressure from dropping too much.
This keeps cerebral blood flow constant when there are changes in blood pressure. It begins to fail when mean arterial blood pressure falls below 50mmHg as vessels cannot dilate any further. This reduction in blood flow causes syncope (fainting).
Metabolic autoregulation
This mechanism also regulates local blood flow to the brain by allowing the blood vessel diameter to change in response to changes in the partial pressure of arterial CO2.
Metabolically active tissues may produce local hypercapnia (raised CO2) when their activity exceeds their blood supply. Hypercapnia causes vasodilation to increase blood flow and supply the tissues that have a higher oxygen demand. Conversely, in hypocapnia (low CO2), vasoconstriction occurs.
Cushing Reflex
Raised intracranial pressure, such as in the case of a cerebral tumour or an intracranial bleed, impairs cerebral circulation as it pushes against blood vessels and compresses their lumens.
This is detected by vasomotor control regions in the brainstem. This triggers an increase in the sympathetic vasomotor activity, resulting in peripheral vasoconstriction, tachycardia (increased heart rate) and increased inotropy (contractile force). This raises the blood pressure, forcing cerebral blood vessels to dilate and maintain adequate blood flow.
The increased blood pressure is detected by baroreceptors (mechanoreceptors which sense changes in arterial pressure) in the aortic arch and carotid sinus. Baroreceptors increase the vagal tone to the sino-atrial (SA) node in the heart. This produces bradycardia (slow heart rate).
Additionally, as the intracranial pressure rises, the brainstem is compressed, resulting in an irregular breathing pattern. Thus a clinical triad (called Cushing’s triad) of hypertension, bradycardia and irregular breathing indicates high intracranial pressure.
Clinical Relevance – Syncope
Syncope (fainting) is when there is a loss of consciousness for a short period followed by sudden regain of consciousness. It is caused by reduced blood flow to the brain. It can be a result of Stokes-Adams syndrome, sick sinus syndrome or panic attacks.
Clinical Relevance – Stokes-Adams attacks
Stokes-Adams syndrome is when there are recurrent episodes of syncope due to the heart being unable to pump enough blood to adequately perfuse the brain. The main cause of this is heart block, which is where the electrical impulse travelling through the heart is impeded. heart block is often secondary to other cardiac conditions, such as myocardial infarction, valvular diseases or cardiomyopathy.
Stokes-Adams syndrome is treated by treating the underlying condition and, in some cases, by a cardiac pacemaker.
Clinical Relevance – Sick sinus syndrome
Sick sinus syndrome is a dysfunction of the sino-atrial (SA) node, often leading to bradycardia and, sometimes, pauses in the heartbeat. This can be due to idiopathic (no known cause) fibrosis of the SA node, or it can be secondary to other cardiac diseases or drugs like digoxin or beta-blockers. Symptoms of sick sinus syndrome include syncope, as well as fatigue and palpitations (increased awareness of heartbeat). In sick sinus syndrome, the cardiac electrical impulse is spontaneously generated by atrial muscle, called ectopic atrial beats. This can lead to bursts of tachycardia between the bradycardia, also known as tachy-brady syndrome.
Similar to Stokes-Adams syndrome, sick sinus syndrome can also be managed by treating the underlying cause or by a cardiac pacemaker
Clinical Relevance – Panic attacks
Panic attacks can cause an individual to hyperventilate. This causes hypocapnia as CO2 is being blown out faster than its production rate. The resulting hypocapnia causes cerebral vasoconstriction via metabolic autoregulation, reducing blood flow (and therefore oxygen and glucose) to the brain. Therefore, the brain tissue is not being perfused sufficiently to maintain consciousness. This causes syncope.
