The hypothalamic-pituitary-gonadal (HPG) axis includes the hypothalamus, pituitary gland and gonads. Gonadotropins are the hormones produced to control the reproductive system.
The hormones involved are gonadotropin-releasing hormone (GnRH) secreted from the hypothalamus, luteinizing hormone (LH) and follicle-stimulating hormone (FSH) produced by the anterior pituitary gland and oestrogen and testosterone produced by the gonads. LH and FSH are known as gonadotropins.
It is essential for the control of the reproductive system and regulates the production of gametes and sex steroids. This article will discuss the function of the HPG axis, its regulation and relevant clinical conditions.
Function of Gonadotropins
Function in Males
Luteinizing Hormone
LH stimulates the Leydig cells in the testes to produce testosterone, the main male sex steroid hormone.
Testosterone has numerous effects, including:
- Stimulates formation of sperm (spermatogenesis) in the testes
- Maintenance of libido (sexual drive)
- Development of secondary sexual characteristics (pubic, axillary and facial hair)
- Growth of external genitalia
- Deepening of voice
- Muscle growth
- Bone growth
- Promotion of anabolic reactions
In some tissues, testosterone is converted to dihydrotestosterone (DHT), making up 10% of total circulating testosterone levels. DHT binds to the same receptors as testosterone. Some tissues only respond to DHT, while others such as the prostate are more sensitive to DHT than testosterone.
High levels of testosterone have a negative feedback effect on the hypothalamus to inhibit GnRH production, as well on gonadotrophs in the pituitary to inhibit LH secretion, thereby decreasing testosterone levels.
Follicle Stimulating Hormone
FSH drives sperm production in the Sertoli cells of the testes (spermatogenesis), as well as synthesis of proteins important for the production and action of steroid hormones. They include:
- Androgen binding protein (ABP) which maintains high levels of testosterone locally in the luminal space of the seminiferous tubules.
- P450 aromatase, an enzyme that converts testosterone into oestradiol.
- Growth factors that support sperm cells and spermatogenesis, that result in increasing the number of sperm cells, as well as promote motility and the fertility potential of sperm.
- Inhibins, which have a selective negative feedback effect on FSH only and not LH (i.e., inhibits FSH production, but does not inhibit LH production). They also act as growth factors on Leydig cells.
Function in Females
LH and FSH stimulate the ovary to produce mature gametes, as well as synthesise and secrete oestrogens and progestins.
LH binds to theca cells on developing follicles as well as granulosa cells. After ovulation, LH binds to cells of the. corpus luteum. It acts on theca cells to produce progestins and androgens. Androgens enter granulosa cells and are then converted to oestrogens.
FSH binds to granulosa cells to:
- Increase production of enzymes that catalyse the production of steroid hormones, stimulating follicle growth
- Increase production of activins, which have a positive feedback effect on the anterior pituitary
- Increase production of inhibins, which have a selective negative feedback effect on the pituitary
- Help convert androgens to oestrogen
Further information on the actions of FSH and LH within the female can be found here.
Feedback Effects in Females
Oestrogens and progestins act on the anterior pituitary and the hypothalamus to exert negative and positive feedback effects.
- Moderate oestrogen levels exert negative feedback on LH and FSH secretion
- High oestrogen levels (in the absence of progesterone) positively feedback on LH and FSH secretion
- Oestrogen in the presence of progesterone exerts negative feedback on the HPG axis
Progesterone is a sex steroid released by the corpus luteum, which is what the follicle turns into after the egg has been released during ovulation.
Progesterone increases the inhibitory effect of moderate oestrogen concentration levels on LH and FSH secretion. However, progesterone prevents the positive feedback effect of high oestrogen concentrations on the pituitary. For more information about how this impacts contraception, click here.
Regulation of The HPG Axis
Gonadotropin-Releasing Hormone (GnRH) is released in a pulsatile fashion from neurons in the hypothalamus. These neurons form an interconnected network with other neural circuits of the brain, allowing for integration of various signals, including light-dark cycles, body fat levels and stress.
GnRH acts on GnRH receptors found on gonadotroph cells of the anterior pituitary, stimulating the production of two hormones:
- Luteinising Hormone (LH)
- Follicle Stimulating Hormone (FSH)
LH and FSH are released in an episodic fashion, reflecting the pulsatile release of GnRH.
LH and FSH then act on the gonads (testes/ovaries), with differential effects.
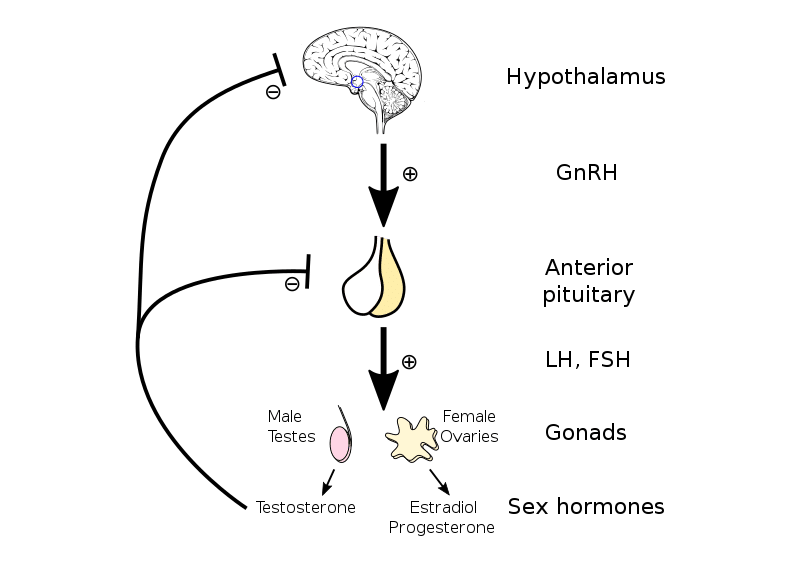
Fig 1 – Diagram showing the HPG axis and its regulation
Clinical Relevance – Prostate Cancer
When GnRH binds to gonadotrophs in the pituitary, the GnRH receptor becomes internalised and degraded by lysosomes. As a result, prolonged and continuous exposure of gonadotrophs to GnRH causes a diminished response and suppresses the release of LH and FSH.
Desensitisation to GnRH can be induced for clinical benefit. In prostate cancer, long-acting GnRH analogues are administered to suppress LH and FSH release, thereby reducing testosterone production. This is effectively medical/chemical castration.
This is useful in the treatment of prostate cancer because testosterone production can cause the cancer to grow, so by removing this signal the tumour will shrink.
