The cough reflex is an important defence mechanism which clears the airways of irritants by forcefully expelling air from the respiratory tract.
This article will discuss the cough reflex arc, its phases and clinical correlations.
Cough Reflex Arc
The cough reflex arc is made up of three main pathways:
Sensory Afferent Pathway
The cough reflex arc is initiated by irritation of cough receptors, for example, mechanoreceptors or chemoreceptors. Irritants are detected by these receptors and they send sensory information to afferent nerves.
There are three main types of sensory nerve fibres involved in the afferent pathway:
- Rapidly Adapting Stretch Receptors (RARs)
- These are myelinated fibres found mostly in the pharynx and trachea which rapidly respond to mechanical stimuli, e.g. changes in lung volumes
- Slowly Adapting Stretch Receptors (SARs)
- These are myelinated fibres which respond more slowly to mechanical stimuli and are involved in the Hering-Breuer reflex
- C-fibres
- These are non-myelinated nerve fibres which respond to mechanical and chemical stimuli
Sensory information travels from these fibres through the afferent pathway via the vagus nerve to the medulla oblongata.
Central Pathway
Sensory information travels to the nucleus tractus solitarius (NTS) of the medulla. The vagus nerve then synapses with motor neurones, delivering information to effector muscles which triggers the cough reflex to occur.
Motor Efferent Pathway
Various respiratory muscles contract to allow initiation of the cough reflex.
- The diaphragm contracts to become flattened which increases the thoracic cavity space
- The laryngeal muscles contract to close the vocal cords
- The external intercostal muscles contract to change the space available in the thoracic cavity
- Rectus abdominis contracts to depress the rib cage and decrease space in the thoracic cavity
Phases of the Cough Reflex
There are three main phases to the cough reflex:
Inspiratory Phase
Irritation of cough receptors causes the vocal cords to open more widely, allowing more air to enter the lungs. The external intercostal muscles and diaphragm then contract causing expansion of the chest cavity, facilitating movement of air into the lungs, and increasing intra-thoracic pressure.
Compression Phase
The epiglottis and vocal cords close, trapping the air within the lungs. There is expiration against the closed epiglottis, causing a further increase in intra-thoracic pressure.
Expiratory Phase
The internal intercostal muscles and abdominal muscles contract to depress the thoracic cavity. The vocal cords relax, and the epiglottis opens. This releases the pressure from the lungs and causes air and the irritant to be rapidly expelled.
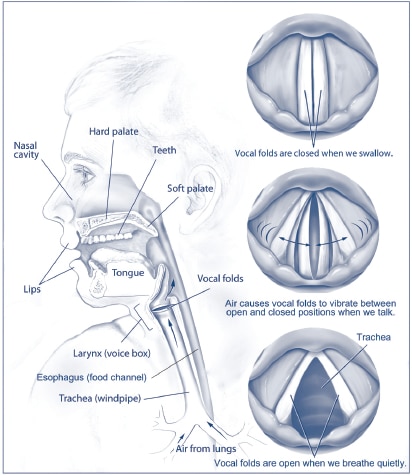
Fig 1 – Diagram showing the upper respiratory system and different positions of the vocal cords.
Clinical Relevance – ACE Inhibitors
ACE inhibitors (Angiotensin Converting Enzyme inhibitors) are commonly prescribed antihypertensive drugs. A common side effect of these is development of a persistent dry cough. This is because ACE inhibitors prevent the inactivation of bradykinin, and cause it to accumulate in the respiratory tract. Bradykinin can cause chemical irritation of the C-fibres of the respiratory tract through the release of proinflammatory peptides (e.g. substance P) and histamine, which results in hyperstimulation of the cough reflex.
