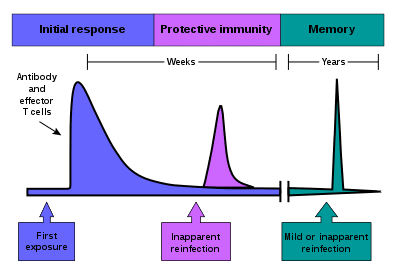
Immunological memory refers to the ability of the immune system to recognise and respond to previously encountered antigens.
In brief, when B and T-cells replicate during the primary immune response, they produce effector cells and long-lived memory cells. Memory B and T-cells are antigen-specific and, on encountering the antigen again, can mount a more rapid and effective immune response, known as the secondary immune response.
This article will discuss memory lymphocytes, active and passive memory, the differences between the two immune responses and finally, clinical correlations.
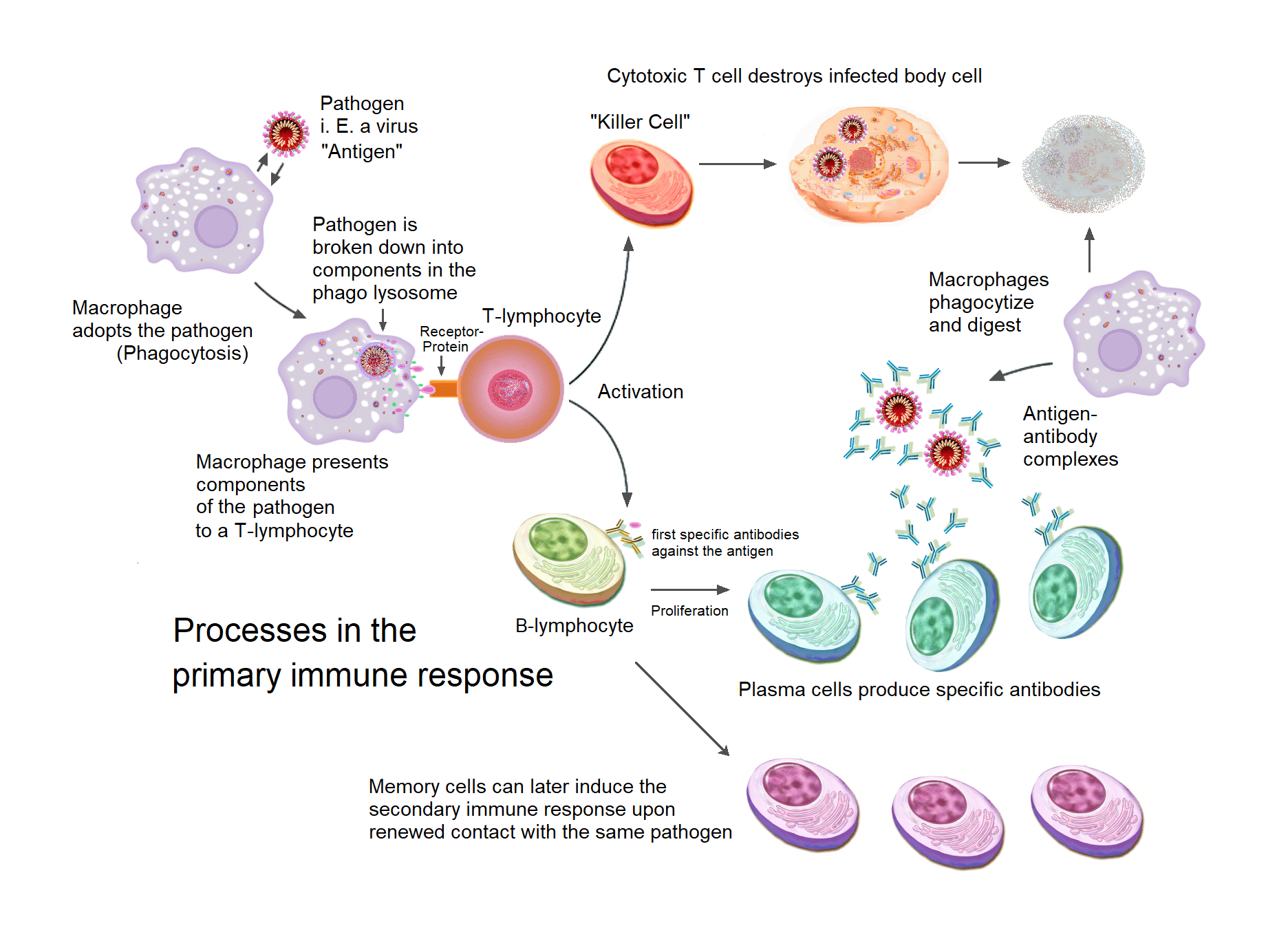
Primary Immune Response
Memory B-cells are long-lived plasma cells that are formed mainly in the germinal centres.
Firstly, during the primary immune response, naïve B-cells are activated by T-cells. after that, B-cells move to secondary lymphoid organs like the spleen and lymph nodes where they enter B-cell follicles or germinal centres within the cortex.
Inside the germinal centre, B-cells proliferate and undergo somatic hypermutation which changes the affinity of their receptor. The receptors are then tested for their affinity within the germinal centre.
In summary, B-cells that can bind their antigens on follicular dendritic cells subsequently receive survival signals from T-cells, while those that do not bind or bind with less affinity are outcompeted and undergo apoptosis. Moreover, B-cells will class switch from IgM to other antibody types such as IgA or IgG.
After somatic hypermutation and class-switching, B-cells differentiate into plasma cells and memory B-cells. Plasma cells are short-lived and die quickly following the primary immune response.
On the other hand, memory cells are long-lived and relocate to the periphery where they are more likely to encounter antigen on re-exposure. Many of the circulating B-cells become concentrated in areas of the body where there is a high likelihood of encountering antigen, such as in Peyer’s patches.
Secondary Immune Response
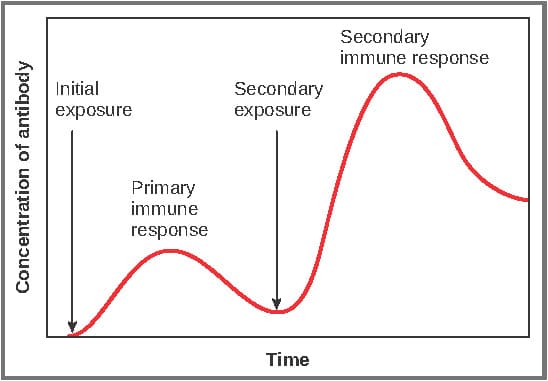
When these memory cells meet their specific antigen again, they rapidly proliferate and differentiate into plasma cells. These plasma cells then respond by producing abundant quantities of antibody to clear the antigen.
A subset of these memory cells can also go into the germinal centres for further class switching and affinity maturation. Memory B-cells can also activate effector T-cells by presenting antigen on MHC-II molecules.
The process of differentiation from memory B-cell to plasma cell is quicker than if they have differentiated from naïve B cells. Memory cells can survive for decades and so can respond to multiple exposures over time. Furthermore, they do not require continual interaction with antigen or T-cells to survive. As they have already undergone class switching and affinity maturation, they can divide faster and produce higher affinity antibodies such as IgG in response to antigen.
Memory T Cells
For memory T-cells, see this page.
Overview of Immune Responses
The table below summarises some key differences between the primary and secondary immune responses:
| Primary immune response | Secondary immune response | |
| Responding cells |
Naïve B and T cells |
Memory B and T cells |
| The threshold for activation (i.e., the dose of antigen needed to initiate response) |
High |
Low |
| Onset of response |
Slow |
Quick |
| Rate of antibody production |
Low |
High |
| Lag phase (time between antigen exposure and antibody detection) |
Long lag phase (4-7 days) |
Short lag phase (1-3 days) |
| Time to peak antibody response |
7-10 days |
3-5 days |
| Antibody types |
IgM >>>IgG |
IgG >>> IgM IgA and IgE may also be present |
| Antibody affinity |
Low-affinity antibodies |
High-affinity antibodies |
| Response magnitude |
Depends on the antigen, but antibody levels are relatively low and decline rapidly |
100-1000x higher than the primary response; antibody titres remain high for longer periods of time |
| Immunity |
Slow control of infection |
Rapid control of infection |
| T cell activation |
Delay before effector T cells are activated |
Effector T cells are present and can act immediately. |
| Innate immune system |
Innate immunity works alone until the adaptive response is initiated |
The adaptive and innate immune system work together from the start |
Clinical Relevance – Vaccinations
The principle of T-cell memory is exploited through vaccinations. A vaccine contains weakened or dead forms of the pathogen and is designed to mimic the initial exposure.
Upon entry, the dead or weakened pathogen is captured and presented on APCs which stimulates the innate immune response. Consequently, this leads to the differentiation of naïve T cells and the expansion of T and B cell populations.
Although there is no clinical infection to fight in this scenario, the vaccine enables the production of T-memory cells so that should a live form of this pathogen enter the body the immune system is already prepared to fight it.