The innate immune system has several first-line barriers to infection, preventing the entry and growth of pathogens.
This article discusses the physical, physiological, chemical, and biological barriers and clinical conditions that may result from their failure.
However, it is important to note that the below barriers work in parallel with various cellular and humoral agents (from both the innate and adaptive immune systems) to prevent colonisation and infection.
Physical Barriers
These barriers provide a physical block against pathogens. The largest barrier comprises the skin, which has a large surface area and covers most of the body’s external surfaces. superficially, the skin has multiple layers of dead, keratinised epithelium which is continuously sloughed off, facilitating the removal of any adherent microbes.
The mucous membranes of the respiratory, gastrointestinal and urinary tracts are also in contact with the external environment. The outermost, epithelial layer is held together by tight junctions, making it robust enough to impede deeper pathogen access.
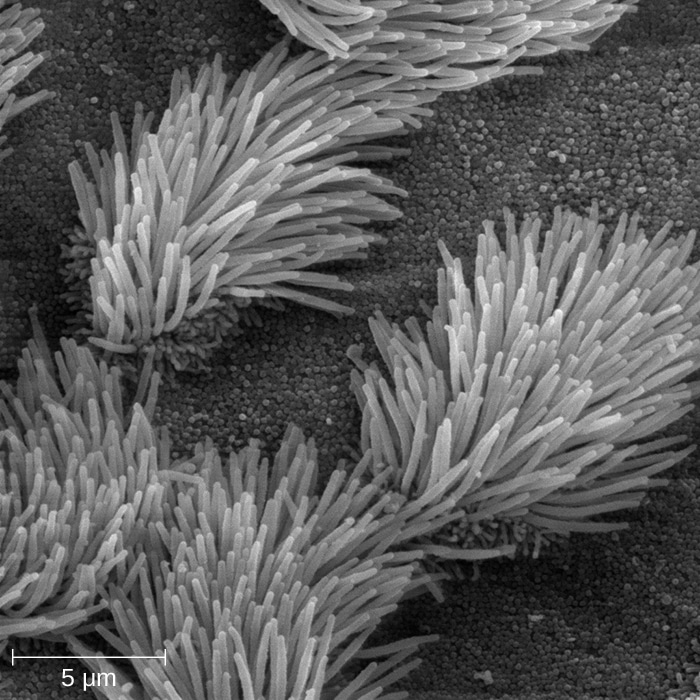
Another physical barrier of the innate system is the bronchial cilia. These cells form the mucociliary escalator, which allows the gradual removal of pathogens from the respiratory system.
Finally, some surfaces are constantly irrigated by various secretions, the components of which will be discussed in more detail below. The free flow and drainage of secretions are important in and of themselves in avoiding infections. Tears, urine, saliva, bile, pancreatic secretions, mucus and sebaceous secretions help protect the surfaces they flow over from infection by reducing pathogenic attachment and duration of contact with bodily surfaces. If the flow is obstructed, the static fluid becomes a nutritious site for infection by various microorganisms.
Clinical Relevance – Ciliary Dysfunction
Kartagener’s syndrome is a recessive genetic disorder characterised by defective cilia movement. Affected individuals have a triad of features: situs inversus, chronic sinusitis, and bronchiectasis.
Disruption of normal cilia function leads to recurrent chest infections, resulting in scarring, dilatation, and distortion of the bronchi – so-called bronchiectasis.
Another important genetic disorder where mucociliary movement becomes deranged is cystic fibrosis. Cystic fibrosis is autosomal recessive and affects multiple organ systems. It results from mutations in the cystic fibrosis transmembrane conductance regulator (CFTR) protein, a chloride channel. The ionic imbalance in CF leads to a change in the consistency of the mucus produced. Thick mucus builds up in different passageways within the body, such as the lungs, and prevents mucociliary clearance. In the airways, this manifests as an increased propensity for infections and breathing difficulties.
Physiological Barriers
The physiological barriers of the body are processes that occur in response to pathogens to remove them from the system and vary depending on location and situation. The main physiological barriers are:
- Diarrhoea
- Vomiting
- Coughing
- Sneezing
Chemical Barriers
Broadly speaking, there are two main chemical barriers to infection. Firstly, there are microenvironmental factors such as pH. The relatively low pH in certain parts of the body prevents pathogen growth. For example, the following areas of the body have an acidic pH:
- Skin – pH 5.5
- Gastric acid – pH 1-3
- Vagina – pH 4.4
These conditions create a hostile environment that pathogens struggle to thrive in and, especially in the case of gastric acid, can directly kill microorganisms by denaturing their proteins.
There are also a variety of innate antimicrobial molecules throughout the body that can aid in the destruction of pathogens:
- IgA – present in tears, saliva, and mucous membranes.
- Lysozyme – Has bactericidal properties; Present in sebum, perspiration, and urine. Paneth cells in the crypts of the small intestine produce lysozymes as well as phospholipase A and defensins (below).
- Mucus – Has antiseptic peptides and works passively to prevent bacterial adhesion. The viscous nature of mucous traps bacteria, which can then be actively cleared by the mucociliary escalator in the lung or peristalsis of the gut. It is present in mucous membranes.
- Defensins – epithelial cells and cells of the innate immune system produce small proteins called defensins. There are many types with various antimicrobial and antifungal properties. However, the main two types found in vertebrates are alpha and beta-defensins. Beta-defensins help epithelial surfaces to resist microbial colonisation. They can kill microbes by creating channels and disrupting the microbial cell membrane. Alpha defensins are found in macrophages, neutrophils, and intestinal paneth cells.
- Enzymes – for example, pepsin is an endopeptidase present in the gastrointestinal tract and can help kill bacteria through proteolysis.
Biological Barriers
The main biological barrier to pathogens is the normal flora found within the body. These are non-pathogenic microbes found within strategic locations of the body – primarily those in contact with the external environment. These are typically found in the:
- Nasopharynx
- Mouth and throat
- Skin
- GI tract
- Vagina
Normal flora consists of non-invasive commensal microorganisms that do not normally cause disease. However, they outcompete pathogens for attachment sites and resources and may even produce antimicrobial chemicals. For example, vaginal bacilli secrete antimicrobial peptides like lactic acid to inhibit pathogenic activity. In addition to this, many also produce essential vitamins, such as Vitamin K and B12.
Loss of normal microbiota is associated with the use of antibiotics or excessive use of antiseptic solutions. This can provide an opportunity for pathogenic bacteria to colonise the vacated tissues. For example, the use of systemic, broad-spectrum antibiotics such as penicillins/cephalosporins lead to alterations in the normal bowel flora. In other words, the treatment kills off the competing, commensal species. This subsequently allows the outgrowth of pathogenic species such as Clostridium difficile which produce harmful toxins, resulting in intestinal inflammation and abdominal symptoms.
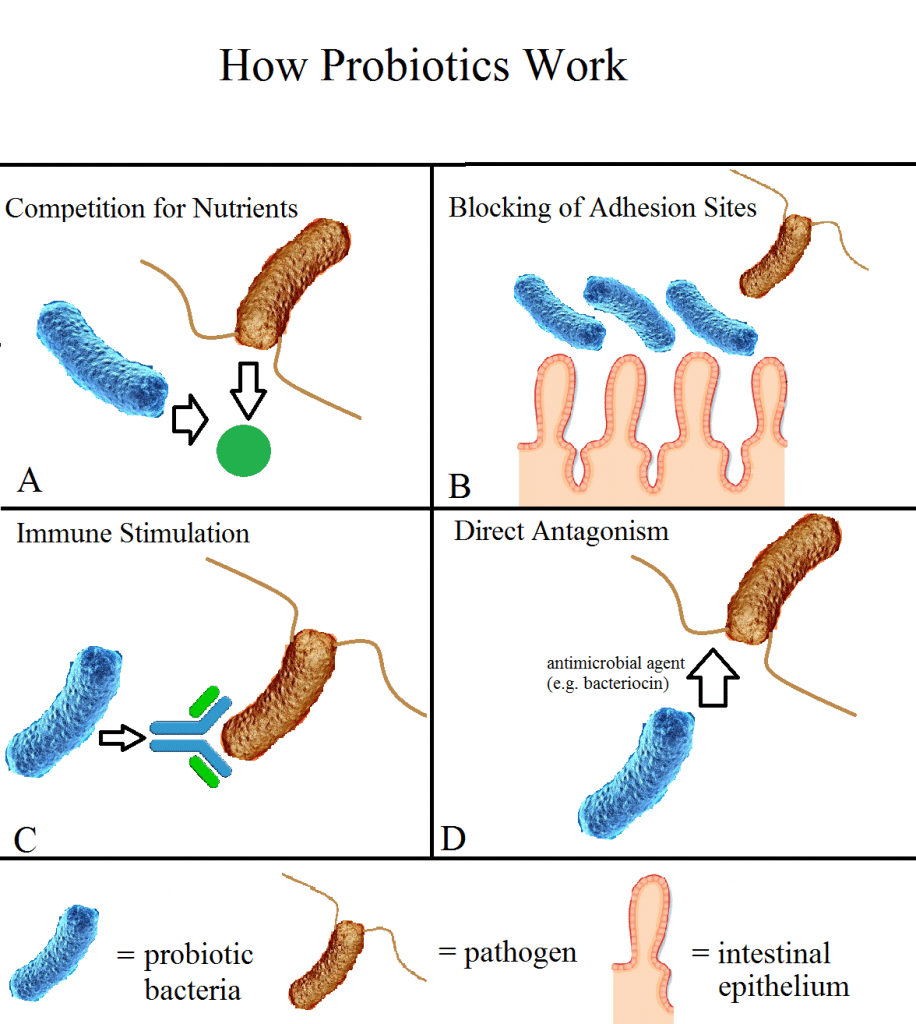
Fig 2 – Mechanisms by which normal flora can prevent infection.
Examples of Normal Flora
| Location | Examples of Normal Flora |
| Conjunctiva | Coagulase-negative Staphylococci
Haemophilus spp. Staphylococcus aureus |
| Nose | Coagulase-negative staphylococci
Viridans streptococci Staphylococcus aureus Neisseria spp. Haemophilus spp. Streptococcus pneumoniae |
| Outer ear | Coagulase-negative staphylococci
Pseudomonas spp. |
| Mouth and oropharynx | Viridans streptococci
Coagulase-negative staphylococci Neisseria spp. Streptococcus pneumoniae Beta-haemolytic streptococci (not group A) Candida spp. Haemophilus spp. |
| Skin | Coagulase-negative staphylococci
Staphylococcus aureus Streptococci (various species) Bacillum spp. Candida spp. |
| Stomach | Streptococcus
Staphylococcus Lactobacillus |
| Small intestine | Lactobacillus spp.
Bacteroides spp. Clostridium spp. Enterococci Enterobacteriaceae |
| Large intestine | Bacteroides spp.
Clostridium spp. Escherichia coli Klebsiella spp. Lactobacillus spp. Enterococci Acinetobacter spp. Proteus spp. |
| Urethra | Coagulase-negative staphylococci
Diphtheroids Streptococci (various species) Mycobacterium spp. Bacteroides spp. |
| Vagina | Lactobacillus spp.
Diphtheroids Clostridium spp. Bacteroides spp. Candida spp. Actinomyces |
Clinical Relevance
Meningitis
Meningitis is an acute infection of the protective membranes covering the brain and spinal cord. In other words, it describes inflammation of the meninges. It can result from a bacterial or viral infection. Although the majority are viral cases, the most common bacterial agent is Neisseria meningitidis. Symptoms include:
- Fever
- Headache
- Neck stiffness
- Confusion
- Altered consciousness
- Vomiting
- Photophobia
Cases caused by meningococcal bacteria may also present with a characteristic, non-blanching rash. Due to the proximity of the infection to the central nervous system, it is classified as a medical emergency.
Meningitis can be diagnosed with a lumbar puncture, but treatment varies depending on the cause. For example, in suspected bacterial meningitis, empirical antibiotics (cephalosporins) should be immediately commenced. In addition to this, supportive therapy such as fluids and corticosteroids may also be given. In severe cases, admission to an intensive care unit may be required, especially in cases with altered consciousness and respiratory failure.