The thyroid gland is an endocrine organ found in the neck, it is responsible for regulating the body’s metabolic rate via hormones it produces. In this article, we will be looking at its anatomy, its cellular structure, its endocrine physiology and its clinical relevance.
Anatomy
The thyroid gland is a ductless alveolar gland found in the anterior neck, just below the laryngeal prominence (Adam’s apple). It is roughly butterfly-shaped, with two lobes wrapping around the trachea and connected in the middle by an isthmus. The thyroid gland is not usually palpable.
It is supplied by superior and inferior thyroid arteries, drained via superior, middle and inferior thyroid veins and has a rich lymphatic system.
You can read more about the anatomy of the Thyroid gland here.
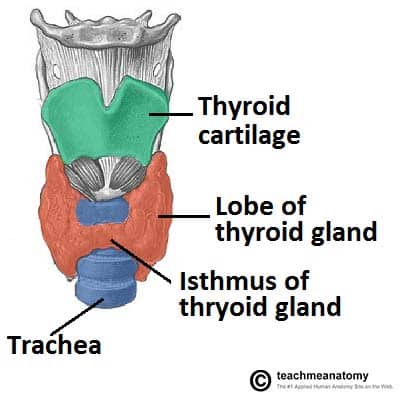
Fig 1 – Anterior view of the neck, showing the anatomical position of the thyroid gland
Cellular Structure
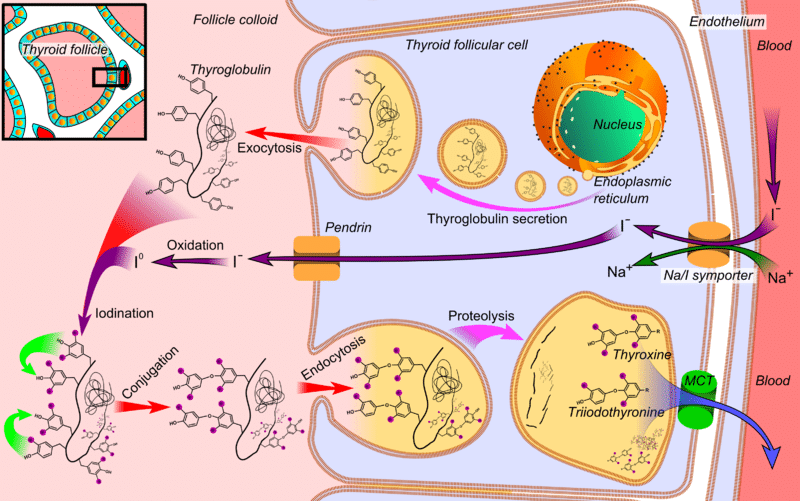
The function of the Thyroid gland is to produce and store thyroid hormones. Thyroid epithelia form follicles filled with colloid – a protein-rich reservoir of the materials needed for thyroid hormone production. These follicles range in size from 0.02-0.3mm and the epithelium may be simple cuboidal or simple columnar.
In the spaces between the follicles, parafollicular cells can be found. These cells secrete calcitonin, which is involved in the regulation of calcium metabolism in the body.
Function
The thyroid gland is one of the main regulators of metabolism. T3 and T4 typically act via nuclear receptors in target tissues and initiate a variety of metabolic pathways. High levels of them typically cause these processes to occur faster or more frequently. Metabolic processes increased by thyroid hormones include:
- Basal Metabolic Rate
- Gluconeogenesis
- Glycogenolysis
- Protein synthesis
- Lipogenesis
- Thermogenesis
This is achieved in a number of ways, such as increasing the size and number of mitochondria within cells, increasing Na-K pump activity and increasing the presence of β-adrenergic receptors in tissues such as cardiac muscle.
Thyroid Hormone Synthesis
There are six steps in the synthesis of thyroid hormone, and you can remember them using the mnemonic ATE ICE:
- Active transport of iodide into the follicular cell via the sodium-iodide symporter (NIS). This is actually secondary active transport, and the sodium gradient driving it is maintained by a sodium-potassium ATPase.
- Thyroglobulin (Tg), a large protein rich in tyrosine, is formed in follicular ribosomes and placed into secretory vesicles.
- Exocytosis of thyroglobulin into the follicle lumen, where it is stored as colloid. Thyroglobulin is the scaffold upon which thyroid hormone is synthesised.
- Iodination of the thyroglobulin. Iodide is made reactive by the enzyme thyroid peroxidase. Iodide binds to the benzene ring on tyrosine residues of thyroglobulin, forming monoiodotyrosine (MIT) then diiodotyrosine (DIT).
- Coupling of MIT and DIT gives the triiodothyronine (T3) hormone and coupling of DIT and DIT gives the tetraiodothyronine (T4) hormone, also known as thyroxine.
- Endocytosis of iodinated thyroglobulin back into the follicular cell. Thyroglobulin undergoes proteolysis in lysosomes to cleave the iodinated tyrosine residues from the larger protein. Free T3 or T4 is then released, and the thyroglobulin scaffold is recycled.
T3 and T4 are the active thyroid hormones. They are fat soluble and mostly carried by plasma proteins – thyronine binding globulin (TBG) and albumin. While T3 is the more potent form, it also has a shorter half-life due to its lower affinity for the binding proteins. Less than 1% of T3 and T4 is unbound free hormone.
At the peripheries, T4 is deiodinated to the more active T3. T3 and T4 are deactivated by removing iodine. This happens in the liver and kidney. As T4 has a longer half-life, it is used in the treatment of hypothyroidism over T3 as its plasma concentrations are easier to manage.
Thyroid Hormone Release
Thyroid hormones are released as part of the hypothalamic-pituitary-thyroid axis. The hypothalamus detects a low plasma concentration of thyroid hormone and releases thyrotropin-releasing hormone (TRH) into the hypophyseal portal system.
TRH binds to receptors found on thyrotrophic cells of the anterior pituitary gland, causing them to release thyroid stimulating hormone (TSH) into the systemic circulation. TSH binds to TSH receptors on the basolateral membrane of thyroid follicular cells and induces the synthesis and release of thyroid hormone.
Clinical Relevance – Thyroid Disorders
Hyperthyroidism
Hyperthyroidism is the medical term for an overactive thyroid gland. One common cause of hyperthyroidism is Grave’s Disease – an autoimmune condition where antibodies are produced that stimulate the TSH receptors on follicular cells. It affects roughly 1% of the population and is 10 times more common in women than in men.
Patients may present with heat intolerance, weight loss, tachycardia, nervousness, increased sweating, exophthalmos and increased bowel movements. Hyperthyroidism can be treated with carbimazole which inhibits iodine binding to thyroglobulin.
Hypothyroidism
Hypothyroidism is an underactive thyroid gland. One common cause of hypothyroidism is Hashimoto’s disease – an autoimmune condition where thyroid follicles are destroyed or antibodies are produced that block the TSH receptor on follicle cells.
Like hyperthyroidism, roughly 1% of the population is affected with it being 10 times more common in women than in men. In the developing world, the most common cause of hypothyroidism is iodine deficiency.
Patients can present with cold intolerance, weight gain, bradycardia, poor concentration, myxoedema, dry skin, some hair loss and constipation. Hypothyroidism can be treated with oral T4 tablets (100-200 µg/day), to replace the hormone that is not being produced by the body.
One way to remember the associated diseases with hyperthyroidism and hypothyroidism is to look at the prominent vowels in each: hypErthyroidism is caused by gravE‘s disease, whereas hypOthyroidism is caused by hashimOtO‘s disease.
Summary
| Table 1 – Clinical features of hyperthyroidism and hypothyroidism | |
| Hyperthyroidism | Hypothyroidism |
| Anxiety | Depression |
| Restlessness | Fatigue |
| Tachycardia | Bradycardia |
| Weight loss | Weight gain |
| Thinning skin | Dry, itchy skin |
| Heat intolerance | Cold intolerance |
| Frequent bowel movements | Constipation |
| Goitre possible | Goitre possible |
| Low TSH | High TSH |
| High T3/T4 | Low T3/T4 |