Peripheral circulation is important for transporting blood around the body and exchanging nutrients with tissues. The variety of tissues in the body and their need for blood and nutrients varies. Therefore, peripheral circulation must match blood flow to tissue demand. This article looks at how flow is regulated through the peripheral circulation.
Physiology of the Cardiovascular System
Oxygenated blood leaves the left side of the heart via the aorta, a large elastic artery. The aorta progressively branches into smaller muscular arteries and thereafter into arterioles and metarterioles, finally ending in capillaries which supply blood to tissue. The pressure drops as we move from the aorta to the capillaries, however, the aorta has minimal resistance to flow compared to the arterioles.
When discussing changes in “total peripheral resistance,” we are effectively looking at the changes taking place within arterioles, often referred to as the resistance vessels of our circulatory system. Such changes allow the body to increase or decrease blood flow to tissues and alter gas exchange as necessary.
Distribution of Blood at Rest
The heart is the driving force of the body and with every heart beat blood is delivered to the arterial tree. The contraction of the heart generates pressure waves, which propel blood around the body. The amount of blood the heart pumps in one minute (the cardiac output) is typically around 5 L/min. This can be calculated using the following equation:
Cardiac output = stroke volume x heart rate
Stroke volume is the volume of blood ejected by the left ventricle with each contraction. As previously discussed, the arterial system is a high-pressure system with low resistance. This high pressure is important in order to allow blood to be pumped through the high resistance present in the arterioles.
If we add up all of the arteriolar resistances, this will give us a value, which we refer to as the total peripheral resistance.
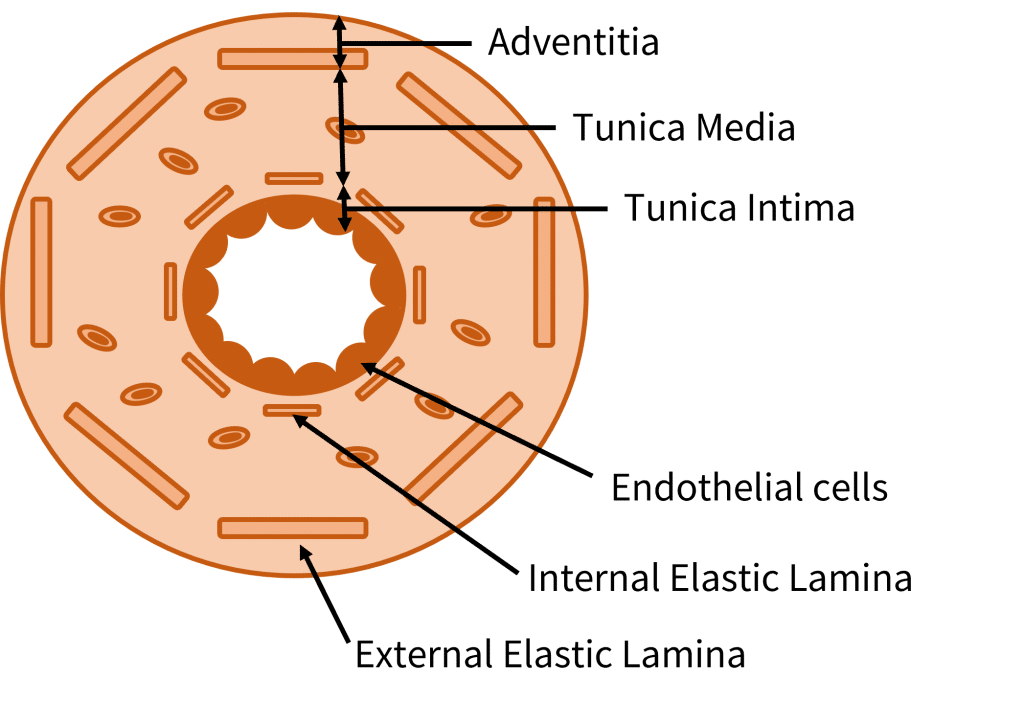
Structure of an Arteriole
An artery with a diameter of less than 0.1mm is called an arteriole. They have a muscular layer, often consisting of a single layer of smooth muscle cells. More information on the anatomy of blood vessels can be found here.
Regulating Arteriolar Tone
By regulating the vasomotor tone of arterioles (amount of tension/contraction of the smooth muscle in the walls), we can control the blood flow to the capillary beds. This is achieved by controlling the vasoconstriction and vasodilation of the arterioles.
At rest, there is a high vasomotor tone i.e. the tonic contraction of the smooth muscle is higher. This is because the tissues require less blood during rest. The sympathetic nervous system is largely responsible for controlling the vasomotor tone. It causes noradrenaline release, which then acts on α1 GPCRs (G-protein coupled receptors).
The vasomotor tone of arterioles can be altered in response to changes in tissue requirements for blood flow. These changes can be brought about by several factors such as vasodilator metabolites, myogenic factors and autocoids.
Vasodilator Metabolites
Metabolically active tissues release vasodilator metabolites such as H+, CO2, K+, adenosine and lactate. These reduce the vasomotor tone by causing vasodilation of the arterioles through smooth muscle relaxation. As the resistance in the arteriole has reduced, the blood flow to the tissue can increase. This is useful as it allows blood to transport metabolites away from tissue, thus helping limit potential toxic effects to tissue. Once the metabolites have been removed, the vasomotor tone will return back to its normal level.
Myogenic Factors
Myogenic factors can also alter vasomotor tone. For example, when the arterioles experience a rapid increase in intraluminal pressure such as due to violent coughing, the arteriolar smooth muscle will contract in order to defend itself from the rise in pressure.
Autocoids
Additionally, the arteriolar endothelium can release biological factors known as autocoids. These behave in a similar way to hormones and can therefore increase or decrease the vasomotor tone.
Clinical Relevance – Reactive Hyperaemia
When there is a lack of blood flow to an area, vasodilator metabolites accumulate in large concentrations. This leads to maximal dilation of arterioles with no blood flow to clear these metabolites as they continue to be produced. As a result, when blood flow returns, resistance is very low and flow is very high. The high blood flow clears the metabolites which leads to the contraction of smooth muscle. This allows blood flow to return to normal.
This often occurs as a consequence of Raynaud’s phenomenon where vasospasm, often triggered by cold or emotional stress, results in ischaemia.