Upper motor neurones make up half of the body’s somatic nervous system – the other half being made of lower motor neurones. Damage to either leads to distinct clinical presentations, allowing the clinician to anatomically pinpoint the location of the damage. In this article, we will consider the definition, function, and clinical significance of the upper motor neurones.
Introduction to UMNs
An upper motor neurone (UMN) is is a neurone whose cell body originates in the cerebral cortex or brainstem and terminates within the brainstem or spinal cord. Therefore neurones that give rise to the various descending motor tracts are all UMNs. In addition, neurones that synapse onto the nuclei of the extrapyramidal tracts (such as the rubrospinal tract) are also UMNs.
Within the clinical practice, the term UMN is typically used to describe descending motor neurones within the corticospinal and corticobulbar tracts. These arise from the pre-central gyrus and terminate in the ventral horn of the spinal cord and motor nuclei of cranial nerves, respectively.
If there is an UMN there must be a lower motor neurone (LMN). You can find out more about LMNs here.
In essence, a UMN will synapse with an LMN, which will synapse onto a muscle (for example). All UMNs exert their effects via LMNs, which may be one singular LMN or several LMNs. In reality, the system is more complicated, with several interneurones acting on both UMNs and LMNs, but the concept is the same. The neurotransmitter typically involved in the transmission from upper to lower motor neurones is glutamate.
Function
This section will focus on the UMNs in the context of the corticospinal and corticobulbar tracts. Both tracts originate within the pre-central gyrus, also known as M1 (primary motor cortex).
The pre-central gyrus is somatotopically organised. This means that particular areas of the body correspond to specific points of the cortex; there is a relationship between where a neurone originates and its function. This gives rise to the motor homunculus, where areas of the body with a larger precision of motor control (eg. the hands) have a larger cortical representation. Likewise, areas which do not have a great deal of motor precision have a smaller representation in the cortex.
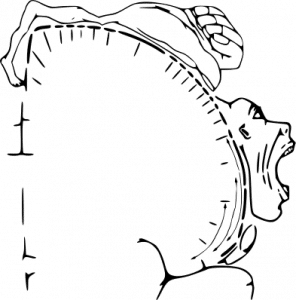
Fig 2 – A 2-D representation of the motor homunculus.
The function of the UMN can be thought of as similar to that of the corticospinal tract i.e. to facilitate voluntary movement. To be more specific, one cortical motor neurone can for example, activate a group of muscles at different times in order to facilitate a certain movement.
Further information on the descending tracts can be found here.
UMN Signs
When an UMN malfunctions a patient displays a variety of specific neurological signs. These signs are known collectively as a UMN syndrome. This distinction is useful as it aids the clinician in discerning where a lesion may be (UMN lesion vs LMN lesion). However, the term does not refer to any specific descending tract being affected.
As expected, damage to an UMN would cause weakness (-paresis) or paralysis (-plegia) of the group of muscles it indirectly innervates. This paresis or paralysis is typically widespread in the form of either a mono/hemiparesis or mono/hemiplegia.
The other functions of UMNs can be understood through observing what other clinical signs occur when they are damaged. These include:
- Hypertonia – UMNs exert a modulatory role in governing muscle tone through what is known as descending inhibition. It is thought that UMNs regulate inhibitory interneurons and their effect on alpha and gamma motor neurones. Loss of UMN input, and thus descending inhibition, means firing of alpha and gamma motor neurones increases, causing hypertonia.
- Hyperreflexia – Descending inhibition from the UMNs also regulates the extent to which the stretch reflex is elicited. Therefore, loss of the UMN activity causes brisk reflexes.
- Spasticity – This describes an increase in the muscle tone on passive movement in a velocity-dependent manner. The amount of resistance felt during the examination is directly proportional to the speed of passive movement. Hence, the faster the muscle is streteched or moved, the greater the resistance to the stretch is felt. In simple terms, on rapid passive movement of a limb, there will be a point where the muscle becomes suddenly resistant to further stretch.
- Positive Babinski sign – The Babinski test is a fundamental component of a neurological examination. The clinician firmly strokes a blunt object along the lateral border of the plantar surface of the foot. A normal response is flexion of the large toe and adduction of the other toes. This is a negative Babinski sign. However, in patients who have an UMN lesion an abnormal plantar reflex is elicited. This is the large toe extends and there is abduction of the other toes. This is a positive Babinski sign. In infants below the age of two, a positive Babinski sign is normal. This is because the corticospinal tracts are not fully developed yet.
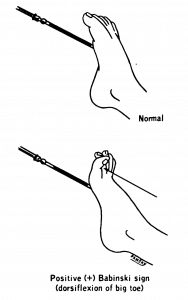
Fig 3 – Negative and positive Babinski’s sign.
- Clonus – this is a series of contractions that occur in a muscle when it is suddenly stretched and held in that position. This likley arises via a reduced descending inhibition, which leads to an exaggerated stretch reflex.
Long-term disuse of a muscle due to paralysis may cause disuse atrophy. It is also important to note that although hypertonia and hyperreflexia are long-term consequences of UMN damage, there is often initial hypotonia and hyporeflexia, immediately following the damage.
Clinical Relevance – Stroke
A stroke, or cerebrovascular event, is a clinical syndrome involving a sudden loss of brain function caused by disruption of the blood supply to the brain. A stroke and a transient ischaemic attack (TIA) differ in duration. In TIA, the neurological disturbances last less than 24 hours and resolve completely in a TIA. In a stroke, the disturbances persist or even result in death. You can read more about strokes here.
Strokes can be broadly divided into two types: ischaemic and haemorrhagic:
- An ischaemic stroke is caused by an obstruction of a blood vessel, which limits the blood flow to the brain substance. The most common cause of this type of stroke are atherothromboemboli from the carotids. In simple terms, a fragment of a carotid atheroma detaches (embolises) and plugs a blood vessel. Other causes also include thrombosis of small vessels or emboli coming directly from the heart.
- A haemorrhagic stroke is caused by a bleed within the brain. The resulting haematoma (a blood collection) exerts a pressure on surrounding brain tissue and impairs its function and blood supply. This type of stroke is caused by intraparenchymal haemorrhage (a bleed within a brain substance) or a subarachnoid haemorrhage, following an aneurysm rupture.
Other rare causes include carotid artery dissection, vasculitis, and venous sinus thrombosis.
Risk Factors
Risk factors for strokes are similar to that of other cardiovascular diseases such as a myocardial infarction. These include:
- Smoking
- Poor diet
- Alcohol
- History of cardiovascular risk factors e.g. hypertension and atrial fibrillation
- Hyperlipidemia
- Diabetes mellitus
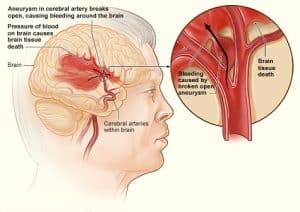
Fig 4 – Haemorrhagic stroke caused by a ruptured aneurysm.
Strokes are a common cause of UMN signs since cranial or brainstem ischaemia affects the function of neurones located in these regions. The clinical signs caused by strokes typically relate to the affected vessel and its respective blood distribution. In particular, UMN signs are seen in total or partial anterior circulation strokes as these affect the motor cortex. In addition, subcortical lacunar strokes of the internal capsule will result in UMN signs.
80% of patients who have a stroke will experience either hemiparesis or hemiplegia, whereas 40% will go on to have long-term impairment of function in the upper limb. Sensory deficits, such as numbness, dysphagia, dysarthria, homonymous hemianopia, and other symptoms may also be present depending on the cerebral vessels that are affected.
It is not uncommon for patients to regain some function in a previously plegic (weakened) limb as the rubrospinal tract is able to compensate for the loss of corticospinal fibres to a certain extent.

