T cells (also called T lymphocytes) are major components of the adaptive immune system. Their roles include directly killing infected host cells, activating other immune cells, producing cytokines, and regulating the immune response.
This article discusses T cell production, the different T cell types, and relevant clinical conditions.
Production of T Cells
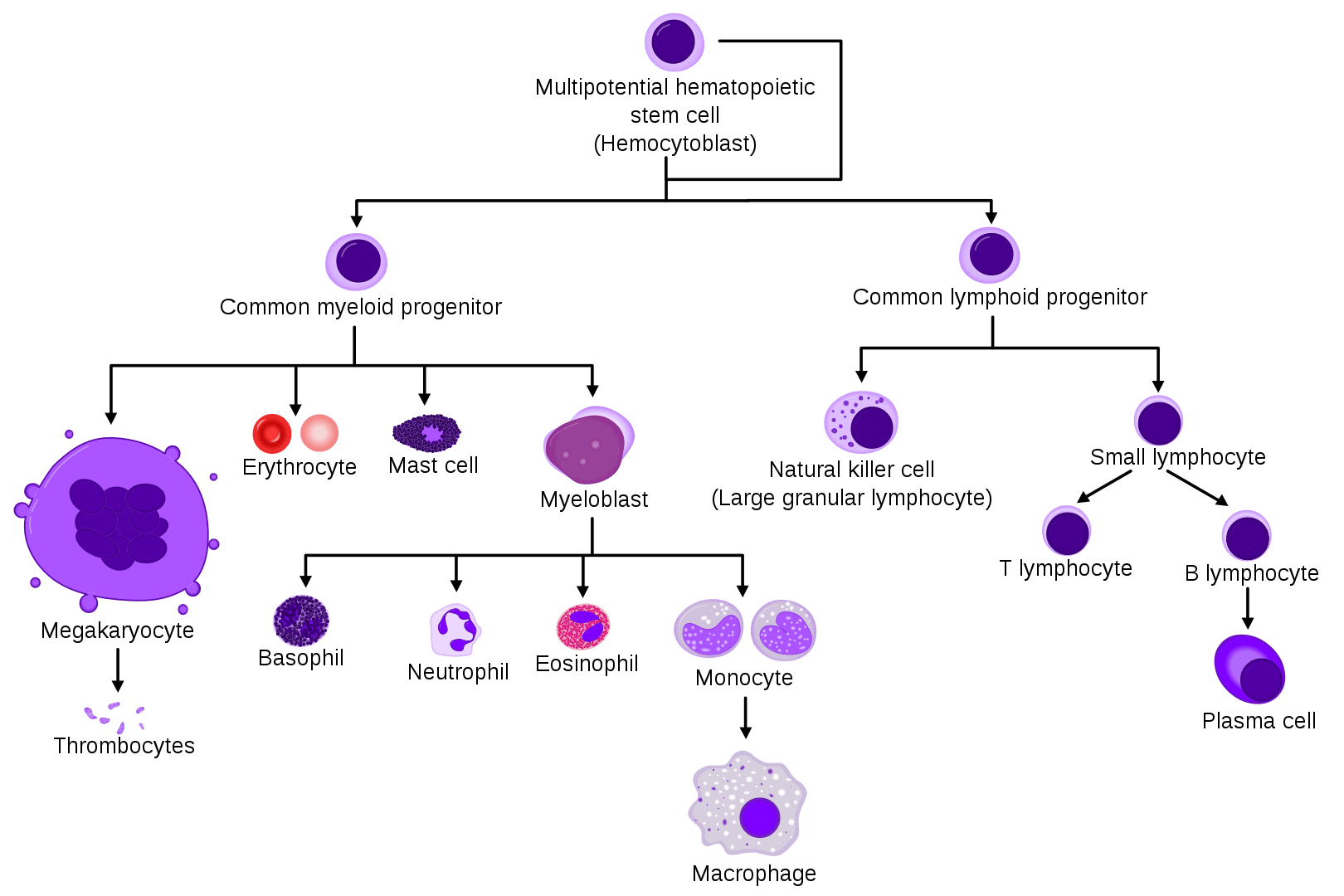
T lymphocytes originate from haematopoietic stem cells within the bone marrow. Some of these multipotent cells subsequently become lymphoid progenitor cells that leave the bone marrow and travel to the thymus via the blood.
Once in the thymus, T lymphocytes undergo a selection process in which the majority of developing T cells (called thymocytes) will not survive. During this process, thymocytes with receptors for self-antigens receive negative signals and are removed from the repertoire.
Each T lymphocyte has a T cell receptor (TCR) which is specific to a particular antigen. T lymphocytes that survive thymic selection will mature and leave the thymus. After that, they circulate through peripheral lymphoid organs, ready to encounter their antigens and become activated. The thymus atrophies as we age and so produces fewer naïve T lymphocytes over time.
T Cell Types
Naïve T lymphocytes are cells that have not yet encountered their specific antigen. In peripheral lymphoid organs, naïve T lymphocytes can interact with antigen-presenting cells (APCs), which use Major Histocompatibility Complex (MHC) molecules to present antigens.
Once the T lymphocytes recognise their specific antigens, they proliferate and differentiate into one of several effector T lymphocyte subsets. Effector T lymphocytes interact with host cells (rather than the pathogen) to carry out their immune function.
T lymphocytes use co-receptors to bind to the MHC molecules. Co-receptors can be either CD4 or CD8. CD proteins help to differentiate major groups of effector T lymphocytes. Naïve CD8+ T lymphocytes will become cytotoxic T lymphocytes and CD4+ T lymphocytes will become T helper lymphocytes, each of which is specialised for particular tasks.
Cytotoxic T Cells
Cytotoxic T lymphocytes kill their target cells by releasing cytotoxic granules into the target cell. These cells recognise their specific antigen (such as fragments of viruses) only when presented on MHC Class I molecules present on the surface of all nucleated cells.
MHC Class I molecules interact with CD8 on the cytotoxic T cells. Cytotoxic T cells require several signals from other cells like dendritic cells and T helper cells to be activated.
Their main function is to kill virally infected cells, but they also kill cells with intracellular bacteria or tumorous cells.
T-Helper Lymphocytes
T-helper cells (Th) have a wide range of effector functions and can differentiate into many different subtypes, such as Th1, Th2, Th17, TfH cells, and regulatory T cells.
They become activated when they are presented with peptide antigens on MHC Class II molecules. These are expressed on the surface of APCs. MHC Class II molecules interact with CD4 on the T helper cells, which helps identify this cell type.
CD4+ T cell functions include activating other immune cells, releasing cytokines, and helping B cells to produce antibodies. They help to shape, activate, and regulate the adaptive immune response.
Memory T Cells
Antigen-specific, long-lived memory T lymphocytes form following an infection. They are important because they can quickly proliferate into large numbers of effector T lymphocytes upon re-exposure to the antigen and have a low threshold for activation.
They provide the immune system with memory against previously encountered antigens. Memory T lymphocytes may either be CD4+ or CD8+.
Fig 2 – Diagram summarising T cell activation.
| Type | Stimulus cytokines | Transcription factor | Function | Effector molecules | Target organisms | |
| CD8 | Cytotoxic T cells | IL-12
IL-18 |
T-bet
Blimp1 |
Kills virus-infected cells. | Granzyme
Perforin TNF-α Fas ligand |
Viruses |
| CD4 | TH1 cells | IL-12
IFN-γ IL-2 |
T-bet | Activates macrophages.
Helps cytotoxic T-cells.
Provides B-cell help for antibody production |
IL-12
IFN-γ IL-2 |
Intracellular (mycobacteria, listeria, leishmania) and extracellular bacteria.
Fungi. |
| TH2 cells | IL-4 | GATA3
STAT6 |
Provide help to B cells for antibody production- especially IgE antibodies.
Activates eosinophils and mast cells. |
IL-4
IL-5 IL-13 |
Helminth
Extracellular Parasites
|
|
| TH17 cells | IL-6
IL-21 TGF-β |
ROR-γT
STAT3 |
Enhance neutrophil response.
Improve epithelial barrier function. |
IL-17
IL-21 IL-22 IL-26 IL-6 |
Extracellular bacteria (e.g. Salmonella enterica) | |
| TFH cells | IL-6
IL-21
|
Bcl6 | Germinal centre formation.
B cell antibody isotype switching.
Antibody affinity maturation.
Enables B cells to develop into plasma cells for Long term humoral immunity |
IL-10
IL-21 IL-4 |
||
| T regulatory cells | TGF-β
|
Foxp3 | Suppresses other immune cells, particularly CD4+ and CD8+ responses. | TGF-β
IL-10 CTLA-4 |
Clinical Relevance – Severe Combined Immune Deficiency (SCID)
SCID is an umbrella term for a group of primary immunodeficiencies with defects in T and B cell numbers and/or function. Individuals with SCID are prone to recurrent infections, sepsis, and failure to thrive.
They will often be well at birth and for the first few weeks of life due to the antibodies passed to them via the placenta, but symptoms tend to develop within the first three to six months of life. Infections are likely to be more frequent, more severe, and more persistent than usual and they may also develop opportunistic infections due to the poor function of their immune system.
SCID can result from defects in many genes, although the most common defect is X-linked.
The best treatment for SCID is a bone marrow transplant. Patients with SCID are also likely to require prophylactic antibiotics, antifungals, and antivirals while undergoing this treatment and may need immunoglobulin replacement therapy lifelong (depending on how successful the bone marrow transplant is at restoring immune function).